A large, international team of rheumatologists, geneticists, hematologists and other researchers has discovered a severe inflammatory syndrome linked to an acquired genetic mutation in the bone marrow of older men. The X-linked syndrome, they found, is caused by a somatic mutation in myeloid stem cells that hobbles the master regulator of a pathway tasked with ridding cells of accumulated protein debris.
They showed that the alteration of this ubiquitylation pathway by a mutation in the UBA1 gene that encodes the ubiquitin-activating (E1) enzyme results in inflamed myeloid blood cells and a variety of clinical symptoms that can masquerade as other disorders. “The overall main message is that we discovered a new disease that was hiding out amongst a variety of clinical diagnoses,” says Peter Grayson, MD, MSc, the study’s co-senior author and a tenure-track investigator at the National Institute of Arthritis and Musculoskeletal and Skin Diseases, Bethesda, Md. “We have theorized for a long time that somatic or acquired mutations may cause rheumatic diseases, but this is really one of the first examples of that actually being identified.”
VEXAS
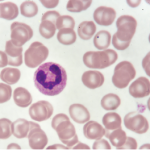
In the new study, published in The New England Journal of Medicine, the researchers dubbed the syndrome VEXAS, after some of its distinguishing features (vacuoles, E1 enzyme, X-linked, autoinflammatory, somatic). Among the 25 men in the study, all had a mutation altering the E1 enzyme’s methionine-41 codon, the start site of a shorter protein isoform that regulates the debris-removal process of ubiquitylation. In VEXAS, the abnormally truncated E1 isoform is enzymatically inactive.
The mutation, Dr. Grayson says, was previously hidden in the data because it appears almost exclusively in myeloid cells and not in lymphocytes. Other genetic diseases have been linked to downstream players in the cellular cleanup process, but the group’s new finding represents one of the first known dysregulations of the master switch. In zebrafish embryos, the team showed a UBA1 gene knockout results in a similar activation of myeloid cells, bolstering the evidence that the mutation causes myeloid-driven inflammation.
‘We knew clinically about patients with systemic inflammatory disease & myelodysplasia; we just didn’t realize that there was a unifying process driving these conditions.’ —Dr. Grayson
Kenneth Warrington, MD, professor of medicine and chair of the division of rheumatology at the Mayo Clinic, Rochester, Minn., hailed the “landmark discovery” as a big step toward understanding the root cause of VEXAS and improving therapeutic interventions. “I think where there is more to be discovered is in how we end up seeing this varied clinical phenotype,” Dr. Warrington says, citing potential interactions with other genes or environmental factors as modulating influences. “It’s obviously not just one gene with one disease, but one gene with a more varied clinical syndrome, which I think, in essence, makes it more interesting and probably why it took so long to identify this.”