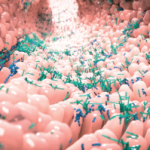
NEW YORK (Reuters Health)—Fluctuations in the gut microbiome over time could underlie inflammatory bowel disease (IBD), including Crohn’s and ulcerative colitis, researchers suggest.
“Both the state and the dynamics of the human gut microbiome in healthy individuals are highly personalized. Although cross-sectional studies have revealed dysbiosis of the gut microbiome in IBD, little is known about the individual nature of microbiome dynamics in IBD,” writes Dr. Janet Jannson of the Earth and Biological Sciences Directorate, Pacific Northwest National Laboratory in Richland, Wash.
Dr. Jannson tells Reuters Health that the study, online Feb. 13 in Nature Microbiology, “is the first to look at the long-term dynamics of different types of IBD.”1
The team analyzed the gut microbiome from an IBD cohort of 137 individuals—49 with Crohn’s disease, including inflammation of the ileum or colon; 60 with ulcerative colitis; four with lymphocytic colitis; 15 with collagenous colitis; and nine healthy controls. They collected one to 10 stool samples per participant at three-month intervals for a total of 683 samples.
“We used a mathematical approach to define a ‘healthy plane’ that described the less volatile dynamics of the gut microbiome in healthy individuals compared to individuals with IBD that deviated from the healthy plane,” Dr. Jannson explains by email.
Samples from patients with colonic Crohn’s disease and ulcerative colitis were closer to the healthy plane, and some samples did not differ significantly from healthy controls.
The gut microbiome of individuals with ileal Crohn’s disease varied most from those of healthy individuals, “with large temporal fluctuations in microbial community composition,” Dr. Jannson observes. The variation was especially noticeable in those who had undergone surgical resection, followed by those who did not undergo surgery.
To address the unequal sampling of healthy individuals vs. IBD patients, the team compared the volatility of their healthy controls with healthy participants in two published studies that used different microbiome project datasets. Across all three cohorts, less volatility was observed in healthy individuals compared with those with IBD.
“Monitoring the gut microbiome is a non-invasive approach, and we found it to be a better predictor of IBD disease phenotype than f-calprotectin measurements or human genetic markers,” Dr. Jannson says. “The results of this study are key to precision medicine because the gut microbiome can be used to guide personalized treatment therapies.”
Coauthor Dr. Jonas Halfvarson of Orebro University in Sweden, tells Reuters Health, “From a clinical perspective, our data demonstrate the complexity of IBD and the need to address the dynamics when exploring mechanisms related to disease etiology of chronic diseases … with periods of remissions and episodes of flares.”
“As a next step, we need more in-depth data,” he says by email. “For example, what are the major drivers of the trajectories, beyond corticosteroids, due to a clinical flare? This requires more frequent sampling. In the end, we are aiming to understand how we could maintain IBD patients in the healthy plane and how this will influence the disease course.”
Gastroenterologist Dr. Louis Cohen of The Mount Sinai Hospital in New York tells Reuters Health, “The individual variability of human microbial ecology makes it difficult to establish meaningful connections between bacterial populations and human health at one time point, making longitudinal studies such as this critical to the understanding of how bacterial ecology can predict disease pathophysiology or contribute to it.”
“The authors put forth an intriguing idea that there exists a healthy distribution of bacteria in stool and this ecology can vary over time to a certain degree,” he says by email.
“The most powerful finding is that perhaps even when in remission, patients with IBD have a highly dynamic bacterial ecology,” he notes. “Whether the instability of the microbiome is secondary to yet unknown confounders such as diet or is actually a meaningful observation about how host-microbial interactions shape the landscape of IBD pathophysiology remains to be determined.”
“The authors also suggest that maintaining IBD patients in a ‘healthy plane’ could prevent disease exacerbations,” Dr. Cohen continues. “While this may hold true, the authors’ own data suggests that IBD patients seem to deviate from this ‘healthy plane’ independent of traditional markers of inflammation like calprotectin. This suggests not a connection, but a disconnection between the healthy plane and inflammation in IBD.”
“Overall, this cohort of IBD patients appears relatively healthy—few patients on TNF inhibitors, generally low calprotectin values – and establishing a more definitive link between the healthy plane and IBD microbial ecology will likely take even more time, patients, and resources,” he observes.
“With that said, this study clearly is blazing the trail forward, laying a foundation for other researchers to build on and better determine how the human microbiome impacts health and disease,” Dr. Cohen concludes.
Reference
- Halfvarson J, Brislawn CJ, Lamendella R, et al. Dynamics of the human gut microbiome in inflammatory bowel disease. Nat Microbiol. 2017 Feb 13;2:17004. doi: 10.1038/nmicrobiol.2017.4.