Because of the frequently asymptomatic nature of the uveitis, profound ocular damage can occur silently. According to guidelines developed by the American Academy of Pediatrics, children with polyarticular and pauciarticular JIA should undergo regular slit-lamp examinations at least every six months. Those who are younger than seven and antinuclear antibody–positive should see an ophthalmologist every three to four months. Those with Still’s disease should have an eye exam annually.12
Intermediate or Panuveitis
Behçet’s syndrome: Behçet’s syndrome is a generalized occlusive vasculopathy of unknown cause. Its classic triad consists of acute iritis with hypopyon, painful oral ulcers, and genital ulceration. The disease is most common in Southeast Asia, the Eastern Mediterranean to Japan, and less common in the United States. In Asians, it is associated with HLA-B51.
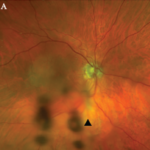
Although Behçet’s syndrome may cause panuveitis, a characteristic feature of this disease is recurrent acute iritis or chronic iridocyclitis. This complication is often bilateral and can be associated with a transient hypopyon. Posterior segment involvement includes retinal vasculitis, retinal hemorrhages, macular edema, focal retinal necrosis, ischemic optic neuropathy, and vitritis.
Treatment of Behçet’s syndrome includes the initial use of oral corticosteroids. Early institution of immunosuppressive medication improves long-term prognosis. Azathioprine and cyclosporine have been shown to be useful treatments in randomized controlled trials. Infliximab and alpha-interferon have shown utility in open-labeled studies. The disease tends to be chronic and recurrent, and—if unsuccessfully treated—can lead to blindness with eventual ischemic retinopathy and optic atrophy.13
Lyme disease: Ocular involvement in Lyme disease occurs at all stages. An early sign is follicular conjunctivitis. Uveitis associated with Lyme disease is rare but could manifest as a chronic iridocyclitis or vitritis.14
Sarcoidosis: Up to half of patients with systemic sarcoidosis exhibit ocular inflammatory diseases and uveitis is the most common ocular manifestation. In most series, sarcoidosis accounts for 3% to 10% of all patients with uveitis evaluated at a referral center.
Sarcoidosis can cause chronic granulomatous iridocyclitis. Typical findings are large keratic precipitates, iris nodules, and white clumps of cells in the inferior anterior vitreous. Iris nodule and posterior synechiae can lead to secondary glaucoma. Posterior segment involvement is less frequent. Small granulomas along retinal venules can be useful in diagnosis. Macular edema and optic disc involvement lead to visual loss. A retinal vasculitis is associated with sarcoidosis even though vasculitis is not typical of this disease in other organs. Ocular disease activity may not parallel other organ manifestations.15