Blau syndrome (familial granulomatous arthritis): Mutations in the human NOD2/CARD15 gene cause Blau syndrome, characterized by granulomatous uveitis, arthritis, and rash. Blau syndrome is an autosomal-dominant disease. Skin rash is usually a prominent initial manifestation, which can be observed in early childhood as painless tiny tan dots. The joint anomalies always appear in the first decade, but do not lead to severe handicap until the fourth or fifth decade of life. Episodes of uveitis tend to recur, and progress to posterior involvement. Uveitis can be associated with disc edema, retinal striae, and secondary glaucoma. Blau syndrome can be mistakenly diagnosed as childhood-onset sarcoidosis, but lack of lung involvement and the mode of inheritance are clues for differentiation.16
Other Rheumatologic Diseases That Cause Uveitis
Cogan’s syndrome: Patients with Cogan’s syndrome present with ocular and audiovestibular symptoms, which typically occur within two years of each other. The most common ocular involvement is bilateral, non-syphilitic interstitial keratitis. Atypical cases can present with scleritis, uveitis, retinitis, and optic neuritis. Audiovestibular symptoms resemble Ménière’s disease. Deafness occurs in about 50% of patients. Systemic manifestations include fever, arthritis, skin rash, lymphadenopathy, gastrointestinal symptoms, neurologic abnormalities, and cardiovascular involvement. Systemic corticosteroids with or without immunosuppressive therapy are often effective in controlling ocular and other visceral manifestations, but have limited success in restoring hearing.17
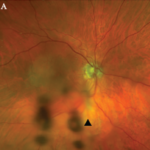
Systemic lupus erythematosus (SLE): Ocular involvement with SLE includes dry eye syndrome, keratitis, scleritis, eyelid lesions, and (rarely) uveitis. The most common intraocular findings are retinal microvascular abnormalities, including cotton-wool spots, retinal arteriolitis, vascular occlusion, and vitreous hemorrhage. The presence of retinal vasculitis and neovascularization often correlates with central nervous system involvement and antiphospholipid antibodies.18
Polyarteritis nodosa: Ocular involvement is rare in polyarteritis nodosa, but includes scleritis, uveitis (iritis and vitritis), hypertensive retinopathy, and retinal vasculitis. Cotton-wool spots and retinal hemorrhages can also be seen. Central retinal artery occlusion and optic atrophy may lead to blindness in the late stage of disease.19
Wegener’s granulomatosis: Eye disease affects 50% of patients with Wegener’s granulomatosis. Common eye findings include orbital inflammation, scleritis, and keratitis. Uveitis as a primary involvement is uncommon. Patients with Wegener’s granulomatosis may develop scleritis as the initial manifestation. Patients with scleritis and a positive antineutrophil cytoplasmic antibody test tend to have severe scleritis, even if other signs of Wegener’s granulomatosis are absent. Posterior scleritis may cause visual loss and ocular pain with exudative retinal detachment. Retinal vasculitis and true retinitis are rarely reported.20,21