Weakness implies a loss of function and a decline in strength, and it is challenging to confirm the absence, rather than the presence, of a symptom.
VasilkovS/shutterstock.com
As clinicians, we are familiar with pain, stiffness and soreness—subjective nouns that define our métier. These helpful words serve as signposts that direct us along the path to the proper diagnosis.
Consider the young man with a stiff, sore back (a case of ankylosing spondylitis?) or the postpartum woman experiencing newly painful, stiff and sore fingers (the onset of rheumatoid arthritis)? How about your patient, the weekend warrior, old enough to have been alive when Woodstock rocked, who now describes feeling stiff and sore around their shoulders and hips (polymyalgia rheumatica, perhaps)? Rheumatologists are accustomed to parsing the meaning of these terms. We are the experts in triaging aches and pains. This is the essence of rheumatology.
But interpreting another nebulous term, weakness, is another story. This noun is among the most vexing descriptors heard when taking a patient’s history, perhaps only matched by the imprecise epithets, feeling dizzy and feeling fatigued. Weakness implies a loss of function, a decline in strength, and it is always challenging to confirm the absence, rather than the presence, of a symptom. Skeletal muscle, unlike its neighboring tissues, the joints, tendons, ligaments and bursae, can silently endure an intense immune attack without raising a whimper. In contrast to all the other –itises, inflammatory myositis is generally a painless event that quietly transforms into a debilitating condition.
Because a steroid-induced myopathy is painless, patients are rarely aware of its stealthy development until the weakness begins to disrupt their lifestyle.
Hiding in Plain Sight
Years ago, some colleagues and I examined a handful of patients who presented with varying complaints of malaise, fatigue and a sense of feeling unwell that led their treating physicians astray. Several patients were noted to have elevated serum liver enzymes that, in combination with their descriptions of malaise and fatigue, led to a liver biopsy in one patient (with normal results) and consideration of this procedure in two others, creating even more diagnostic confusion. It was only when a couple of our astute fellows considered another potential source for these enzyme elevations, namely muscle, and measured the patients’ serum creatine kinase levels that the diagnosis of, what we later termed, occult myositis became evident.1
Idiopathic inflammatory myopathies (IIM), such as polymyositis and dermatomyositis, can arrive with little fanfare. Occasionally, a telltale reddish scaly skin eruption may be present or a wholly unwelcome coincidental paraneoplastic event may occur, but generally, these muscle disorders may simmer along quietly, at least for a while, evading detection. After the diagnosis is made and treatment initiated, other challenges may present, such as determining whether any persistent weakness is a manifestation of ongoing muscle inflammation requiring more aggressive immunosuppression or is an expected consequence of prior muscle damage.
It has been observed that muscle weakness correlates poorly with the inflammatory cell infiltrates detected in muscle biopsies, suggesting that non-immune cell-mediated mechanisms may play a key role in causing weakness in patients with IIM.2 What could these be?
One consideration is that the endoplasmic reticulum (ER) stress response triggered by myositis can create intramuscular havoc by altering the cellular respiration of myocytes, leading to an overproduction of reactive oxygen species. These chemicals can be noxious to the cells’ work engines, the ER and the mitochondria. Any alterations to these organelles may disrupt the proper flow of calcium or potassium ions across specialized channels that is required to generate the energy for muscle contraction to occur. Without contraction, there is no strength. Yet in some patients with myositis, this physiologic injury may persist even in the absence of active muscle inflammation creating management challenges for the treating clinician.
Another conundrum arises when patients treated with glucocorticoids develop proximal muscle weakness. Because a steroid-induced myopathy is painless, patients are rarely aware of its stealthy development until the weakness begins to disrupt their lifestyle. Is their underlying illness getting worse and in need of even higher doses of steroids, or are steroids the culprit for their loss of strength? If we don’t ask the right questions, we may fail to identify the proper cause. The lack of diagnostic blood tests or imaging studies adds to the challenge.
Steroid-induced myopathy, first described in 1932 by Harvey Cushing, MD, in patients afflicted with the disease carrying his name, is thought to be mediated via a toxic effect of corticosteroids on muscle tissue.3 However, we know little about its pathogenesis, save for the finding of type II muscle fiber atrophy left in its wake. Sadly, steroid-induced myopathy has long been neglected by researchers; it’s been well over 30 years since the publication of any novel research in this field.
Yes, weakness can be alarmingly insidious. Years ago, I assumed the care of a middle-aged woman diagnosed with lupus who was becoming progressively weaker over the course of several months. She knew that she was slowing down; her gait was impaired, and she began to stumble and frequently fall. She felt sluggish. A patron of the arts, her world shrank as she became homebound. Her rheumatologist began prescribing monthly courses of intravenous cyclophosphamide and bolus doses of steroids to supplement her daily dose of that drug in the belief that she was developing motor weakness due to an underlying peripheral neuropathy caused by her lupus. Yet, her weakness only worsened.
When I first met Betty, now wheelchair bound, she could barely recount her history. “I am just too tired to talk, doctor. Can I come back another day?”
Something was amiss; her extreme somnolence and lethargy, her deepening voice could not be linked to lupus. The mystery was solved when her circulating serum thyroxine level was barely detectable and her serum thyroid-stimulating hormone level returned in the stratospheric range, 250 units (normal up to 5 units): a classic example of a functioning endocrine feedback loop. Betty was, literally, hours away from descending into myxedema coma.
Many months later, following Betty’s recovery, it became evident that her prior diagnosis of lupus was in error. Her weakness, lethargy, full facies, thinning hair, general malaise and positive ANA masqueraded as lupus when, in fact, these findings could all be attributed to another autoimmune disorder: hypothyroidism caused by Hashimoto’s disease that had annihilated her thyroid gland years earlier. Although she had taken thyroxine for years, it was mistakenly discontinued when she changed primary care doctors. She was advised that it was no longer required—a near fatal error.
The thyroid–muscle interaction can be double edged. A sluggish or an overactive thyroid gland can profoundly influence muscle strength. The latter holds true for thyrotoxic periodic paralysis, a disorder observed in about 15% of Asian men with hyperthyroidism characterized by the abrupt onset of hypokalemia and paralysis primarily affecting the legs.4 Patients are literally stopped in their tracks until the episode of profound weakness resolves.
My brush with this illness occurred years ago when, as a medical resident, I examined a Korean postdoctoral mathematics student who was referred to neurology clinic for his episodic weakness. Living on a tight budget, he described a weekly ritual of consuming as many as six bowls of pasta every Tuesday night at a neighborhood all-you-can-eat restaurant, and he noticed that he would be unable to rise out of bed every Wednesday morning. He adapted to the situation by lying in bed for about an hour, patiently solving quadratic equations, waiting for his legs to recover so that he could start moving again.
The high-carbohydrate load of bowls of pasta can trigger a surfeit of insulin secretion that in turn stimulates excess Na+/K+ ATPase activity in muscle cells, causing a dramatic drop in potassium that renders the muscles dysfunctional.4 Next time, may I suggest a bowl of kimchi?
Muscle & Bone
Our skeletons influence our strength. It has long been observed that osteomalacia due to severe vitamin D deficiency can be associated with weakness. Similarly, patients with cancer that has metastasized to bone are often weaker than one would expect based on the skeletal location of their lesions. Why?
Bone is a rich storehouse of growth factors, including activin A, TGF-beta, IGF-I and BMP-2, that not only have activity in bone as a part of normal remodeling but can impact other organs, including muscle. It is possible that during hyperactive bone resorption, as occurs in metastatic cancer, bone might have a predominant role over muscle in bone–muscle cross-talk and become a source of osteokines that affect muscle function. This has been demonstrated in a murine model of metastatic breast cancer that described a reduction in the strength of paw grip in the absence of tumor involvement of these muscles.5 Likewise, factors released from muscle, such as IGF-I, FGF-2, myostatin and IL-6, may play a critical role in bone metabolism that could further augment the role of bone in muscle dysfunction.
Can Weakness Cause Illness?
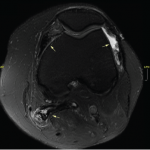
Is it possible for weakness to mediate disease rather than serve as its unwanted end result? The answer to this intriguing question may be at the heart of the pathogenesis of osteoarthritis (OA) of the knee. A thoughtful review of this topic by some of our colleagues summarized the data demonstrating that muscle weakness may be a predictor of the onset of knee OA, but its role in the progression of OA is less clear.6 A few pilot exercise studies have suggested a benefit for some patients at risk for knee OA because it may delay its onset, but exercise has not been shown to impact established OA.
Aging Muscles—Fighting Back
Despite the mixed results for exercise in the management of knee OA, it remains a great alternative to the option of doing nothing. Aging begets the loss of muscle, sarcopenia and, if left unopposed, weakness becomes an inevitability. Fight back with exercise.
For encouragement, look to those aging athletes who continue to excel at their advanced ages: the 85-year-old sub-four-hour marathon runner or the 105-year-old cyclist who continues to pedal at an impressive 14 mph.7,8 Their secret to success is their continued devotion to training and exercise. But for those who are not interested in dripping sweat, there are a few intriguing options that may help one regain one’s strength.
By combining one of humankind’s oldest technologies, textile processing in the form of weaving and knitting, with new advanced materials, such as electroactive polymers, a new form of textile actuator has been developed. These are mass-fabricated, wearable textiles that can scale up force through their design that allows for greater stretch and flexibility. Coupled with tiny electrodes, these wearable materials may eventually provide a power boost to weakened muscles that enables the wearer to perform tasks with greater ease.9
A novel area of weakness research focuses not on muscle, but on the brain. A recent study tested the hypothesis that the cerebral cortex is a critical determinant of muscle strength and weakness and that a high level of corticospinal inhibition is an important neurophysiological factor regulating force generation.9
A group of healthy individuals underwent four weeks of wrist–hand immobilization to induce weakness. Another group also underwent four weeks of immobilization, but they were trained in mindfulness, performing mental imagery exercises of strong muscle contractions five days per week. Mental imagery has been shown to activate several cortical areas that are involved with actual motor behaviors, and in this study, this activity attenuated the loss of strength by half.
Mind over muscle? I wish it were true.
 Simon M. Helfgott, MD, is associate professor of medicine in the Division of Rheumatology, Immunology and Allergy at Harvard Medical School in Boston.
Simon M. Helfgott, MD, is associate professor of medicine in the Division of Rheumatology, Immunology and Allergy at Harvard Medical School in Boston.
References
- Helfgott SM, Karlson E, Beckman E. Misinterpretation of serum transaminase elevations in ‘occult’ myositis. Am J Med. 1993 Oct;95(4):447–449.
- Lightfoot AP, Nagaraju K, McArdle A, et al. Understanding the origin of non-immune cell-mediated weakness in the idiopathic inflammatory myopathies – potential role of ER stress pathways. Curr Opin Rheumatol. 2015 Nov;27(6):580–585.
- Cushing H. The basophil adenomas of the pituitary body and their clinical manifestation (pituitary basophilism). Bulletin of the Johns Hopkins Hospital. 1932;50:137–195.
- Vijayakumar A, Ashwath G, Thimmappa D. Thyrotoxic periodic paralysis: Clinical challenges. Jo J Thyroid Res. 2014;2014:649502.
- Waning DL, Guise TA. Molecular mechanisms of bone metastasis and associated muscle weakness. Clin Cancer Res. 2014 Jun 15;20(12):3071–3077.
- Roos EM, Herzog W, Block JA, et al. Muscle weakness, afferent sensory dysfunction and exercise in knee osteoarthritis. Nat Rev Rheumatol. 2011 Jan;7(1):57–63.
- Longman J. 85-year-old marathoner is so fast that even scientists marvel. The New York Times. 2016 Dec 28.
- Associated Press. 105-year-old Frenchman rides 14 miles in a hour to set world record. ESPN. 2017 Jan 4.
- Clark BC, Mahato NK, Nakazawa M, et al. The power of the mind: The cortex as a critical determinant of muscle strength/weakness. J Neurophysiol. 2014 Dec 15;112(12):3219–3226.