Yet, the biggest difference in diagnosis between pediatric and adult arthritis lies elsewhere: the differential diagnosis (see Table 2. In an adult with joint pain, the major alternatives are usually osteoarthritis, crystalline disease, overuse injuries such as tendonitis or bursitis, and pain amplification syndromes. While patellofemoral syndrome is common in both children and adults, as is pain amplification beginning in early adolescence, most of these other diagnoses are extremely rare in childhood. Their place in the differential diagnosis is assumed by benign hypermobility syndrome, growing pains, transient synovitis of the hip, and diseases specific for the immature skeleton. These latter include Legg-Calvé-Perthes disease (avascular necrosis) of the hip, Osgood-Schlatter syndrome (tibial tuberosity apophysitis) at the knee, and Sever’s disease (calcaneal apophysitis) at the ankle.
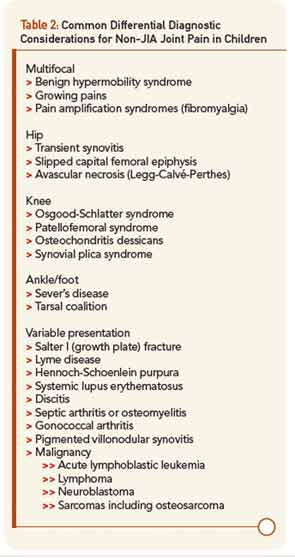
Of greatest clinical concern are diseases affecting the growth plates, which in children may be more vulnerable to injury than ligaments and calcified bone. By far the most important of these is slipped capital femoral epiphysis (SCFE), in which the growth plate of the head of the femur is disrupted leading to anatomic deformity, avascular necrosis, and early hip osteoarthritis. Pain in SCFE is often referred to the knee, so even more than in adults, if the knee hurts, be sure to examine the hip, too. Overall, when evaluating a child with musculoskeletal issues, remember than most of what hurts is not arthritis, while arthritis may not seem to hurt much at all, presenting instead as functional limitation such as limp.3
A word about pain amplification syndromes (the fibromyalgia family). These syndromes are at least as prevalent in the adolescent population as true arthritis.3 As in adults, suspect pain amplification when symptoms and functional limitation are greatly out of proportion to physical and laboratory findings. In the pediatric population, such dysfunction typically presents as school absenteeism. An adolescent with joint pain, fatigue, normal labs, and months of school absence is highly unlikely to have JIA and much more likely to have pain amplification, potentially complicated by issues such as learning disabilities, bullying, depression, and physical or sexual abuse. As in adults, a positive diagnosis spares unnecessary testing and intervention while opening the way to appropriate therapy.
Don’t Forget the Eyes!
For reasons that remain unknown, JIA may be accompanied by destructive inflammation of the eyes, termed chronic anterior uveitis. The major risk factors are young age at onset and a positive ANA titer at any level above normal, with a risk peaking in excess of 30% in some subgroups. Ocular inflammation is usually clinically invisible without a slit lamp, and young children and parents will not notice the problem even as the eye is developing irreversible scarring injury. Therefore, ophthalmological screening should be part of the initial evaluation of suspected JIA, and should continue every three to 12 months depending on risk factors, since the prognosis of the eye depends on the presence or absence of scar at the time uveitis is diagnosed.4 Patients with sJIA, RF-positive poly-JIA, and ERA are generally less susceptible to this complication, though patients with ERA may develop acute anterior uveitis.


