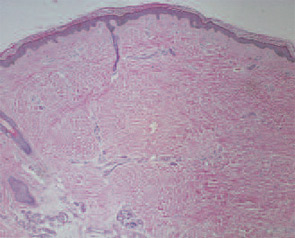
Several groups have reported additional cases of NSF developing in patients with stage 5 chronic kidney disease following exposure to gadodiamide contrast during MR imaging.19-21 When my colleagues and I examined a subcohort of 90 of the 186 patients that we had characterized, for whom active electronic medical records with records of radiologic studies were available, we found a strong association between prior exposure to gadolinium-containing contrast agents and the development of cutaneous changes of NSF. In this study, there was a relative risk of 10.7 for developing the skin changes after gadolinium exposure.18 In light of this new information, a re-review of Endicott’s hospital records revealed that she had undergone MR imaging with gadodiamide the month before she began to develop skin changes of NSF.
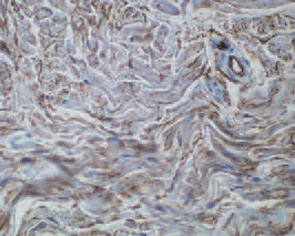
Gadolinium, a rare earth metal, is extremely toxic in its free form. When used as a contrast agent for MR imaging, gadolinium is chelated with one of several organic molecules that trap the gadolinium atom and prevent it from binding to tissues.22 Since 1988, five gadolinium-containing contrast agents have been approved by the Food and Drug Administration for use in MR imaging in the United States. No contrast agent is approved for use in MR angiography. However, gadolinium-containing contrast agents have been used off-label for MR angiography with increasing frequency since 1997, and the appearance of NSF has coincided with this off-label use. Gadodiamide is the least stable of the five gadolinium-containing contrast agents that are available in the United States and therefore is the most likely one to release free gadolinium. Indeed, gadolinium has been detected in skin and blood vessels of patients with NSF who have received gadodiamide.23,24 A contrast agent administered by a radiologist is the only way a patient may be exposed to gadolinium.
Because there is not yet an effective medical treatment to reverse the changes of NSF, patients should receive physical therapy with active and passive range-of-motion exercises to improve or prevent worsening of existing joint contractures. Extracorporeal photopheresis, plasmapheresis, and high-dose intravenous immunoglobulin are expensive modalities and available data do not support their consistent efficacy in treating NSF.
The strong association between NSF and prior exposure to gadolinium-containing contrast agents suggests that this condition might be prevented by not exposing patients with chronic kidney disease to gadolinium. Loma Linda University Medical Center (Calif.) has instituted and published a policy regarding the use of gadolinium-containing contrast agents in patients with chronic kidney disease.19 (See “Guidelines for Using Gadolinium Contrast Agents in Chronic Kidney Disease Patients,”)
