With respect to the role of leptin in RA, leptin serum levels are higher in active disease. Furthermore, the differences in leptin levels between plasma and synovial fluid were greater in nonerosive than in erosive arthritis, supporting the idea of a joint-protective role. However, studies have indicated that known antirheumatic treatments, such as anti-TNF therapy of RA patients, do not influence concentrations of leptin in serum. To elucidate fully the role of leptin in clinical immunology and rheumatology, compartment-related analyses still need to be performed.
The differences in leptin levels between plasma and synovial fluid were greater in nonerosive than in erosive arthritis, supporting the idea of a joint-protective role.
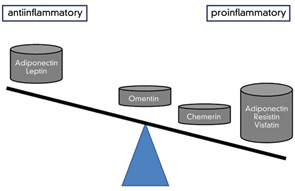
Usually, the effect of proinflammatory signalling molecules does not differ extensively in the various rheumatic diseases. Does this other dogma also hold true for adipokines?
Given that the differential diagnosis of a mild RA versus active osteoarthritis (OA) can be difficult, the identification of a disease-specific adipokine in this setting would be of value. Although studies addressing the role of adipokines in OA are limited, increased adiponectin serum levels appear to be associated with erosive OA, and serum levels have been found to be increased in comparison to healthy individuals. Moreover, visfatin was able to upregulate proinflammatory prostaglandin E2 release in murine arthritis, most likely via activation of the canonical IL-1-chondrocyte-matrix-metalloproteinase pathway.
A similar issue on the role of adipokines in disease exists for the spondyloarthropathies, in which inflammation parameters are generally low and not very useful for (differential) diagnosis. Here, serum levels of resistin in ankylosing spondylitis (AS) patients were found to be low, but nevertheless greater than those in patients with OA. In contrast to the findings with resistin, studies on AS patients showed lower leptin levels compared with controls even after adjustment for body fat mass. These findings suggest a lack of the assumed protective leptin effect. “Fatty life” is complicated. However, in another study, leptin exerted proinflammatory effects on PBMCs from patients with AS, and stimulation of PBMCs from AS patients with exogenous leptin significantly increased IL-6 and TNF production in a dose-dependent manner.15 These findings point to a more direct role of leptin in driving inflammation. (See Figure 3)
Adipokines in Connective Tissue Diseases and Vasculitides
As the dedicated reader might expect, the pathophysiology of connective tissue diseases and vasculitides, especially of systemic lupus erythematosus (SLE), includes also a potential role of adiponectin. In SLE patients with inflammatory glomerulonephritis, the adiponectin isoforms appear to exert different roles, as full-length adiponectin, containing all isoforms except the globular adiponectin–induced IL-8 and monocyte chemotactic protein 1 in microvascular endothelial cells and monocytes. Similarly, studies have indicated that resistin is related to systemic inflammation in SLE. In contrast, the role of leptin in SLE is linked to hypoandrogenicity, reflected by a negative correlation to androstenedione levels.