Management Dilemmas
Although there are few prospective data to guide therapeutic decision making, it is clear that not all patients with CTD-ILD require treatment. We believe whether to treat a patient with CTD-ILD depends on the severity and pace of the ILD and which comorbid conditions or contraindications to treatment exist. Therapy for CTD-ILD is generally reserved for patients with clinically significant, progressive disease. When considering immunomodulatory therapy options for CTD-ILD, both intra- and extrathoracic disease manifestations need to be taken into consideration. Because multiple systems may be affected by CTD, coordinated care among rheumatologists and other subspecialists can be helpful. Although extrathoracic manifestations may determine the initial immunomodulatory regimen, quite often, it is the ILD that dictates the intensity (i.e., specific agent and duration) of the immunosuppressive therapy.
We believe patients with CTD-ILD require a multidisciplinary approach to management, and the challenges in diagnosing, classifying, and treating CTD-ILD create opportunities ripe for carefully planned research.
We are in desperate need of better therapies for CTD-ILD. Determining which drugs are effective for patients with CTD-ILD will require the completion of thoughtfully constructed and carefully conducted large-scale therapeutic trials. Until then, we have to rely on data from small case series or retrospective studies, scientific rationale, and inferences drawn from the few controlled clinical trials conducted for SSc-ILD.
ILD is a serious, potentially life-threatening manifestation of CTD. Patients with all forms of CTD are at risk for developing ILD, and ILD may be the first or only manifestation of a CTD. There are numerous challenges and opportunities related to the clinical care and research of CTD-ILD. We believe patients with CTD-ILD require a multidisciplinary approach to management, and the challenges in diagnosing, classifying, and treating CTD-ILD create opportunities ripe for carefully planned research.
Disclosures
Drs. Fischer and Swigris are investigators for the NIH-funded Scleroderma Lung Study II. Dr. Fischer is a speaker, consultant, and advisory board member for Actelion pharmaceuticals and a speaker and advisory board member for Gilead pharmaceuticals.
Dr. Fischer is associate professor of medicine, acting chief of the division of rheumatology, and in the autoimmune and interstitial lung disease program at National Jewish Health in Denver. Dr. Swigris is associate professor of medicine and in the autoimmune and interstitial lung disease program at National Jewish Health.
References
- Fischer A, West SG, Swigris JJ, et al. Connective tissue disease-associated interstitial lung disease: A call for clarification. Chest. 2010;138:251-256.
- Frankel SK, Brown KK. Collagen vascular diseases of the lung. Clin Pulm Med. 2006;13:25-36.
- Joint Statement of the American Thoracic Society and European Respiratory Society. American Thoracic Society/European Respiratory Society international multidisciplinary consensus classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2002;165:277-304.
- Bouros D, Wells AU, Nicholson AG, et al. Histopathologic subsets of fibrosing alveolitis in patients with systemic sclerosis and their relationship to outcome. Am J Respir Crit Care Med. 2002;165:1581-1586.
- Fischer A, Swigris JJ, Groshong SD, et al. Clinically significant interstitial lung disease in limited scleroderma: Histopathology, clinical features, and survival. Chest. 2008;134:601-605.
- Kim DS, Yoo B, Lee JS, et al. The major histopathologic pattern of pulmonary fibrosis in scleroderma is nonspecific interstitial pneumonia. Sarcoidosis Vasc Diffuse Lung Dis. 2002;19:121-127.
- Lee HK, Kim DS, Yoo B, et al. Histopathologic pattern and clinical features of rheumatoid arthritis-associated interstitial lung disease. Chest. 2005;127:2019-2027.
- Park JH, Kim DS, Park IN, et al. Prognosis of fibrotic interstitial pneumonia: Idiopathic versus collagen vascular disease-related subtypes. Am J Respir Crit Care Med. 2007;175:705-711.
- Kocheril SV, Appleton BE, Somers EC, et al. Comparison of disease progression and mortality of connective tissue disease-related interstitial lung disease and idiopathic interstitial pneumonia. Arthritis Rheum. 2005;53:549-557.
- Hunninghake GW, Zimmerman MB, Schwartz DA, et al. Utility of a lung biopsy for the diagnosis of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2001;164:193-196.
- Kim EJ, Collard HR, King TE, Jr. Rheumatoid arthritis-associated interstitial lung disease: The relevance of histopathologic and radiographic pattern. Chest. 2009; 136:1397-1405.
- Song JW, Do KH, Kim MY, et al. Pathologic and radiologic differences between idiopathic and collagen vascular disease-related usual interstitial pneumonia. Chest. 2009;136:23-30.
- Corte TJ, Copley SJ, Desai SR, et al. Significance of connective tissue disease features in idiopathic interstitial pneumonia. Eur Respir J. 2012;39:661-668.
- Mosca M, Neri R, Bombardieri S. Undifferentiated connective tissue diseases (UCTD): A review of the literature and a proposal for preliminary classification criteria. Clin Exp Rheumatol. 1999;17:615-620.
- Kinder BW, Collard HR, Koth L, et al. Idiopathic nonspecific interstitial pneumonia: Lung manifestation of undifferentiated connective tissue disease? Am J Respir Crit Care Med. 2007;176:691-697.
- Vij R, Noth I, Strek ME. Autoimmune-featured interstitial lung disease: A distinct entity. Chest. 2011;140:1292-1299.
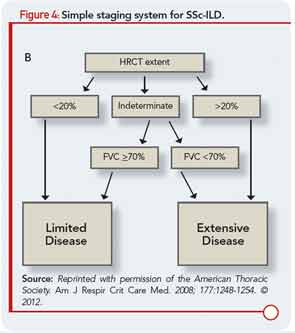
- Goh NS, Desai SR, Veeraraghavan S, et al. Interstitial lung disease in systemic sclerosis: A simple staging system. Am J Respir Crit Care Med. 2008;177:1248-1254.