AL amyloidosis is generally seen in the elderly and rarely occurs in patients under the age of 40.3 Its occurrence is skewed toward males at a nearly 3:1 ratio, as compared to females. Overall, however, the incidence of amyloidosis is relatively low—only about 2,200 new cases are diagnosed in the U.S. annually. That said, the mortality of this disease is significant; without treatment, the median survival is 13.4 months; survival at 5 years is 7%; and 10-year survival rate is a dismal 1%.4
Of patients with AL amyloidosis, those with peripheral neuropathic involvement fare the best and those with cardiac involvement the worst. “The typical cause of death in a patient with systemic AL amyloidosis is congestive heart failure due to massive infiltration of the heart with amyloid,” said Dr. Kay.
Clinical Features
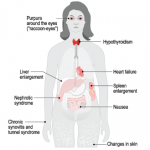
The clinical features of amyloidosis range from vague to striking. “Patients may present with relatively nonspecific symptoms,” Dr. Kay said. “Weakness, fatigue, unexplained weight loss.”
The possibility of fibromyalgia syndrome might first come to mind. However, if present, other obvious clinical features of the disease should prompt a more detailed patient evaluation. These may include waxy papules on the skin surface due to amyloid deposits or nonthrombocytopenic purpura, explained by amyloid deposits binding to clotting factor X, which results in hemorrhages in the skin.
Other features to look for include the otherwise unexplained occurrence of:
- Musculoskeletal
- Noninflammatory arthropathy (“shoulder pads” related to AL, Aβ2M)
- Subcutaneous nodules
- Carpal tunnel syndrome
- Bone cysts
- Destructive spondylarthropathy
- Neurologic
- Sensory neuropathy
- Autonomic neuropathy
- Carpal tunnel syndrome
- Renal
- Proteinuria and/or nephrotic syndrome
- Cardiac
- Congestive heart failure
- Restrictive cardiomyopathy
- Arrhythmias
- Angina
- Pulmonary
- Solitary nodules
- Interstitial infiltration
- Gastrointestinal
- Macroglossia
- Malabsorption
- Diarrhea
- Obstruction
- Ulceration
- Hemorrhage
- Hepatomegaly
- Lymphoid
- Splenomegaly
- Lymphadenopathy
Regarding arthropathy, “In the 1980s, if you walked into a dialysis unit and looked only at the patients’ shoulders … they resembled the hypertrophied deltoid muscles of body builders,” commented Dr. Kay. This was caused by amyloid infiltration of the rotator cuff and surrounding tissues.
(For a more comprehensive review of amyloidosis clinical features, see: Gertz et al. Mayo Clin Proc. 1999;74:490-494.)
Diagnosing Amyloidosis
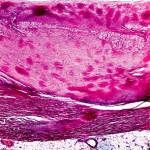
If one or more clinical features are present, a screening biopsy should be performed and stained with the diazo dye, Congo red. Source tissue for biopsy may include bone marrow, rectal tissue, labial salivary gland, or abdominal fat pad aspiration. Dr. Kay described the process of taking an abdominal fat pad biopsy:
Using a 20-cc syringe with a wide-bore, 14- or 16-gauge needle, first draw sterile saline into the syringe. “This allows you to inject, and withdraw [a volume] repeatedly in order to disrupt the abdominal fat globules,” he said. Then aspirate firmly to draw fat globules into the syringe, and deposit the globules on a glass slide. “Place a second slide on top of that,” he explained, “and squeeze to flatten the fat globules. Allow the preparation to air dry and then send it to the pathology department for fixation and Congo red staining.”