The large vessel vasculitides were a major focus of the 21st International Vasculitis Workshop held in Barcelona in April. The biennial conference brings together specialists from multiple disciplines, including rheumatology, nephrology and immunology, to discuss cutting-edge vasculitis research. This article reviews important points regarding the pathogenesis, diagnosis and management of both giant cell arteritis and Takayasu arteritis.1
The large vessel vasculitides were a major focus of the 21st International Vasculitis Workshop held in Barcelona in April. The biennial conference brings together specialists from multiple disciplines, including rheumatology, nephrology and immunology, to discuss cutting-edge vasculitis research. This article reviews important points regarding the pathogenesis, diagnosis and management of both giant cell arteritis and Takayasu arteritis.1
1. Interleukin-17 and giant cell arteritis. Hélène Greigert, André Ramon, Baptiste Lamarthée, et al. Abstract O-005.
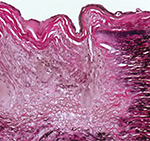
Although giant cell arteritis (GCA) is the most common form of systemic vasculitis in North America, our understanding of its pathogenesis is incomplete. Investigators from Dijon University Hospital and l’Université Bourgogne Franche-Comté, Dijon, France, ascertained the role of interleukin (IL) 17 in the pathogenesis of GCA using two different approaches.
In the first approach, fragments of temporal artery biopsies were cultured in the presence of IL-17, a monoclonal antibody directed against IL-17 (i.e., secukinumab) or pooled immunoglobulin. Using reverse transcription–polymerase chain reaction (RT-PCR), these investigators demonstrated that culturing temporal artery biopsies with IL-17 increased the expression of genes associated with vascular inflammation, T cell recruitment and fibroblast proliferation. However, culturing temporal artery biopsies with secukinumab decreased expression of many of these genes.
In the second approach, vascular myofibroblasts were isolated from healthy arteries and treated with IL-17, interferon-૪, secukinumab or a combinations of these agents, with the following results:
- Interferon-૪ induced expression of IL-17;
- IL-17 induced expression of genes related to vascular inflammation, leukocyte adhesion, and myofibroblast proliferation; and
- These changes were abrogated by exposure to secukinumab.
TitAIN was a phase 2 randomized controlled trial that demonstrated secukinumab may be an effective therapy for giant cell arteritis. This current study provides a mechanistic basis supporting the use of IL-17 blockade for the treatment of giant cell arteritis. Taken together with other studies (see abstract 2603, the evidence suggests secukinumab may become the treatment of choice for patients with giant cell arteritis who fail to respond to tocilizumab.2
2. Infections and incidence of giant cell arteritis. Lucas Pacoureau, François Barde, Alexis Elbaz, et al. Abstract O-014.
The etiology of giant cell arteritis is unclear. However, genetic associations imply that infection may play a role.
In this study, investigators analyzed a cohort of almost 100,000 women who have been followed since 1990. This cohort included 428 patients who had giant cell arteritis and/or polymyalgia rheumatica, who were compared with 8,560 matched controls.
Patients with giant cell arteritis had a higher risk of infection, which was most pronounced in the six months prior to their diagnosis of giant cell arteritis (odds ratio [OR] 1.62, 95% confidence interval [CI] 1.09–2.42). The same increased risk of infection was not observed among patients who had polymyalgia rheumatica alone.
An examination of a claims reimbursement database demonstrated an association between incident giant cell arteritis and recent prescriptions for a fluoroquinolone (OR 2.21, 95% CI 1.12–4.09).
These results support the results of an older study, which observed that the incidence of giant cell arteritis is subject to periodic peaks, just like an epidemic infection.3 However, attempts at identifying a specific culprit agent have failed to yield a promising candidate. Possibly, this may imply that giant cell arteritis can be caused by multiple, unrelated pathogens that induce the same immune response.
The observation linking the onset of giant cell arteritis with prescriptions for fluoroquinolones is a new piece of the puzzle. However, because fluoroquinolones are used for a broad range of indications, the number of potential pathogens remains vast.
3. FDG-PET in patients with giant cell arteritis on tocilizumab. Kaitlin Quinn, Mark Ahlman, Peter Grayson. Abstract O-096.
Tocilizumab has rapidly become part of the standard of care for the treatment of giant cell arteritis. However, tocilizumab also suppresses the acute phase reactants (e.g., erythrocyte sedimentation rate, C-reactive protein) used to track disease activity, further complicating the management of patients with giant cell arteritis treated with tocilizumab.
Quinn et al. identified 31 patients with giant cell arteritis who had achieved clinical disease remission following treatment with tocilizumab for at least six months. Fluorodeoxyglucosepositron emission tomography (FDG-PET) was performed after a median disease duration of 1,070 days, following treatment with tocilizumab for a median of 254 days (interquartile range 189–558).
FDG-PET demonstrated disease activity in 55% of patients. However, none of these patients demonstrated angiographic progression of their vasculitis. Five of the 17 patients who had stopped tocilizumab experienced a disease relapse a median of 1.3 years following drug discontinuation. However, FDG-PET did not demonstrate disease activity in two of these five patients.
Recently updated recommendations from EULAR suggest using imaging studies, such as FDG-PET, to assess for disease activity among patients with giant cell arteritis treated with tocilizumab.4 Notably, Quinn et al. used an FDG-PET scanning protocol optimized for detecting vascular inflammation, including prolonged signal acquisition times, which is not yet standard in most facilities. Despite this, they were unable to demonstrate that FDG-PET was useful for predicting either disease progression or relapse in this patient population.
4. Gastrointestinal perforation in patients with giant cell arteritis on tocilizumab. Desh Nepal, Sebastian Sattui, Zachary Wallace, Michael Putman. Abstract P-055.
Gastrointestinal perforation has been associated with tocilizumab, particularly among patients with a history of diverticulitis. Because diverticular disease is common in an elderly population, many clinicians hesitate to use tocilizumab for patients diagnosed with giant cell arteritis.
In this retrospective study, the TriNetX electronic health records database was used to identify 5,142 patients with giant cell arteritis, 16% of whom received treatment with tocilizumab. Incident gastrointestinal perforations among patients with giant cell arteritis treated with tocilizumab occurred at a rate of 2.0 per 1,000 person-years. Among patients with giant cell arteritis not treated with tocilizumab, the incidence rate was 3.4 per 1,000 person-years.
Gastrointestinal perforation was associated with diverticular disease (relative risk 3.51) and intravenous methylprednisolone (relative risk 5.41). However, when the dataset was used to emulate a clinical trial, using a clone-censor-weight approach that attempts to eliminates the influence of glucocorticoids on the outcome of interest, tocilizumab exposure was not associated with an increased risk of gastrointestinal perforation (hazard ratio 1.05).
Patients with giant cell arteritis who are deemed to be at high risk of poor outcomes are more likely to be treated with both high-dose, intravenous glucocorticoids and tocilizumab. Clinically, therefore, it is difficult to tease apart the relationship between each of these interventions and various untoward events, including gastrointestinal perforation. This novel analysis implies that among patients with giant cell arteritis, high-dose glucocorticoids may largely be to blame for the increased risk of gastrointestinal perforation attributed to tocilizumab. Reassuringly, this study confirms that the overall risk of gastrointestinal perforation among patients with giant cell arteritis is low, whether or not they receive tocilizumab therapy.
5. Spondyloarthritis-spectrum disorders and Takayasu arteritis. Kerem Abacar, Sema Kaymaz-Tahra, Özün Bayındır, et al. Abstract O-078.
Takayasu arteritis is the archetypal large vessel vasculitis, which is associated with a granulomatous inflammation of the aorta and major arterial branches. Takayasu arteritis can also be associated with extravascular manifestations, including retinopathy and arthritis.
Abacar et al. reviewed 350 patients with Takayasu arteritis followed in 12 clinics in Turkey for evidence of disease manifestations associated with HLA-B27. Of these patients, eight (2.2%) had inflammatory bowel disease, eight (2.2%) had psoriasis and 20 (5.7%) had axial spondyloarthritis. Patients with these diagnoses had similar patterns of vascular involvement when compared with patients who had Takayasu arteritis but lacked these features. However, patients with these additional diagnoses tended to develop evidence of Takayasu arteritis at a younger age (26 vs. 32 years old).
This study indicates that patients with inflammatory bowel disease, psoriasis or axial spondyloarthritis may be at increased risk of developing Takayasu arteritis, and increased clinical surveillance required by the spondylitis-spectrum disorder leads to an earlier diagnosis of vasculitis.
This study did not address whether patients with Takayasu arteritis and a spondyloarthritis-spectrum disorder need to be treated more aggressively, although it did note a higher rate of biologic use among these patients. However, this study implies that it may be worthwhile to screen patients with Takayasu arteritis for evidence of inflammatory bowel disease, psoriasis, and ankylosing spondylitis, although the absolute frequency of overlap between Takayasu arteritis and HLA-B27 associated diseases is low.
 Philip Seo, MD, MHS, is an associate professor of medicine at Johns Hopkins University School of Medicine. He served as the third physician editor of The Rheumatologist.
Philip Seo, MD, MHS, is an associate professor of medicine at Johns Hopkins University School of Medicine. He served as the third physician editor of The Rheumatologist.
Author’s note: The 22nd International Vasculitis Workshop will be hosted by the Australia and New Zealand Vasculitis Society Feb. 21–25, 2026, in Melbourne, Australia.
References
- Abstracts book, version 3. 21st International Vasculitis Workshop. 2024 Apr 5.
- Redmond C, Zorc R, Sylvester M, et al. Impact of IL-6 receptor small nucleotide polymorphism Asp358Ala on T cell activity and clinical outcomes in patients with giant cell arteritis [abstract]. Arthritis Rheumatol. 2023;75(suppl 9).
- Salvarani C, Gabriel SE, O’Fallon WM, Hunder GG. The incidence of giant cell arteritis in Olmsted County, Minnesota: Apparent fluctuations in a cyclic pattern. Ann Intern Med. 1995 Aug 1;123(3):192–194.
- Dejaco C, Ramiro S, Bond M, et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice: 2023 update. Ann Rheum Dis. 2024;83:741–751.