Signs of CVID include multiple bacterial or viral infections in a short period of time, poor response to antibiotics, reduced immunoglobulin levels and reduced immune response after vaccinations. But an enormous variation may exist between these patients, said Dr. Gershwin. Cytopenia, bronchiectasis or granuloma, other inflammation or autoimmune diseases are other clues. And in 17.4% of patients, CVID diagnosis comes after the autoimmunity diagnosis.
“There’s no correlation between the presence of autoimmune phenomena in a patient with CVID and its severity,” which may have to do with the genetic basis of the disease, he said. CVID appears both in young children and adults and is a diagnosis of exclusion that is often delayed for years.
In CVID, patients may have a multiplicity of immune cell defects, and each person has different symptoms, complications and disease progression, said Dr. Gershwin. “Perhaps this syndrome, more than almost any other immune deficiency, reflects that it is variable, because it is not one disorder. It represents a multiplicity of disorders all sharing one thing in common: inefficient production of antibodies accompanied by recurrent infections. As we begin to unravel the genetic basis of this disease, individualized, personalized therapy will hopefully improve for these patients.”
Cheaper DNA sequencing has led to the identification of more genetic defects in CVID, but clearly complex, interconnected pathways are at play that are both epigenetic and Mendelian in origin, he said. Although 90% of CVID patients manifest with infections, between 26–30% have autoimmunity.
“So what’s the link? The defect may be closely related to a common susceptibility locus, and it could be that a persistent, opportunistic infection leads by way of molecular mutation that may skew the body toward either a Th1 or Th2 response,” said Dr Gershwin. “There may be incomplete clearance of a pathogen that ultimately leads to some deviation from the immune system or an increased load of apoptosis, leading to an abnormal antigen presentation, increased immune complexes, bystander activation and, ultimately, autoimmunity.”
Multiple familial and environmental factors may influence the immune system in CVID, noted Dr. Gershwin.
“It’s possible that the defect that causes CVID may tilt the immune system toward loss of tolerance and breach of tolerance,” he said. “I can’t give you the reason why someone with primary immune deficiency ends up with autoimmunity. What I can tell you: In patients with CVID, a common variable is abnormal B cell homeostasis.”
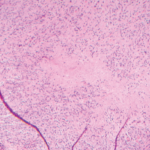
Abnormal B cell function leads to loss of tolerance and reduced autoantibodies in these patients, who also, often, have lymphopenia, expansion of CD8 T lymphocytes and reduced thymic output.