CHICAGO – Presenters at “Looking Ahead to Kinase Inhibition in Rheumatoid Arthritis” delved into some of the big questions that rheumatology faces with kinase inhibitor use.
The presentation, a session here at the 2011 ACR/ARHP Annual Scientific Meeting held in Chicago in November, gave an overview of the kinase inhibitors currently under investigation. [Editor’s note: This session was recorded and is available via ACR SessionSelect at www.rheumatology.org.]
Mark Genovese, MD, professor of medicine and co-chief of the division of immunology and rheumatology at Stanford University in Stanford, Calif., focused on which kinase pathways are important in rheumatoid arthritis (RA) and how researchers decide what to target.
“The reality is that it takes good and complex medicinal chemistry followed by in vitro, animal models, and, ultimately, target validation in humans, and a certain degree of luck,” Dr. Genovese said.
He specifically discussed inhibition of janus (JAK), spleen tyrosine kinase (Syk), phosphodiesterase-4, Bruton’s tyrosine kinase, and phosphoinositide 3-kinase.
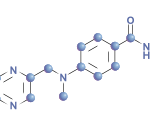
Tofacitinib (CP-690550, Pfizer), a JAK kinase inhibitor, is an oral drug for RA that is currently in phase III trials. Studies have examined tofacitinib as monotherapy or combination therapy dosed twice a day. Research has examined dosing ranging from 5 mg to 30 mg. “In the clinical domain, [JAK inhibitors] have been studied in transplants, RA, psoriasis, inflammatory bowel disease, and myelofibrosis,” said Michael E. Weinblatt, MD, John R. Riedman Professor of Medicine in the division of rheumatology, immunology, and allergy at Brigham and Womens Hospital in Boston.
Presenters at the session said trials show that tofacitinib appears to be an effective treatment for RA. “We know tofacitinib is clinically effective and improves patient function and health-related quality of life in disease-modifying antirheumatic drug [DMARD]–incomplete therapies as monotherapy, with methotrexate and other DMARDs, and is comparable to adalimumab in methotrexate inadequate response,” said Roy Fleischmann, MD, clinical professor in the department of internal medicine at the University of Texas Southwestern Medical School in Dallas.
What is not yet known is whether an optimal dose of tofacitinib will be 5 mg or 10 mg, whether the drug requires methotrexate to be effective, whether tofacitinib’s effects are clinically the same as methotrexate’s or better, and whether the drug is more likely to inhibit radiographic progression, Dr. Fleischmann said.
“If a patient fails to achieve response to 5 mg, will they respond to 10 mg? What if they respond well to 10 mg—will the patient respond to 5 mg? If a patient goes into true remission with tofacitinib, can it be withdrawn, and will the patient maintain the same benefit?” Dr. Fleischmann asked.