CHICAGO – Presenters at “Looking Ahead to Kinase Inhibition in Rheumatoid Arthritis” delved into some of the big questions that rheumatology faces with kinase inhibitor use.
The presentation, a session here at the 2011 ACR/ARHP Annual Scientific Meeting held in Chicago in November, gave an overview of the kinase inhibitors currently under investigation. [Editor’s note: This session was recorded and is available via ACR SessionSelect at www.rheumatology.org.]
Mark Genovese, MD, professor of medicine and co-chief of the division of immunology and rheumatology at Stanford University in Stanford, Calif., focused on which kinase pathways are important in rheumatoid arthritis (RA) and how researchers decide what to target.
“The reality is that it takes good and complex medicinal chemistry followed by in vitro, animal models, and, ultimately, target validation in humans, and a certain degree of luck,” Dr. Genovese said.
He specifically discussed inhibition of janus (JAK), spleen tyrosine kinase (Syk), phosphodiesterase-4, Bruton’s tyrosine kinase, and phosphoinositide 3-kinase.
Tofacitinib (CP-690550, Pfizer), a JAK kinase inhibitor, is an oral drug for RA that is currently in phase III trials. Studies have examined tofacitinib as monotherapy or combination therapy dosed twice a day. Research has examined dosing ranging from 5 mg to 30 mg. “In the clinical domain, [JAK inhibitors] have been studied in transplants, RA, psoriasis, inflammatory bowel disease, and myelofibrosis,” said Michael E. Weinblatt, MD, John R. Riedman Professor of Medicine in the division of rheumatology, immunology, and allergy at Brigham and Womens Hospital in Boston.
Presenters at the session said trials show that tofacitinib appears to be an effective treatment for RA. “We know tofacitinib is clinically effective and improves patient function and health-related quality of life in disease-modifying antirheumatic drug [DMARD]–incomplete therapies as monotherapy, with methotrexate and other DMARDs, and is comparable to adalimumab in methotrexate inadequate response,” said Roy Fleischmann, MD, clinical professor in the department of internal medicine at the University of Texas Southwestern Medical School in Dallas.
What is not yet known is whether an optimal dose of tofacitinib will be 5 mg or 10 mg, whether the drug requires methotrexate to be effective, whether tofacitinib’s effects are clinically the same as methotrexate’s or better, and whether the drug is more likely to inhibit radiographic progression, Dr. Fleischmann said.
“If a patient fails to achieve response to 5 mg, will they respond to 10 mg? What if they respond well to 10 mg—will the patient respond to 5 mg? If a patient goes into true remission with tofacitinib, can it be withdrawn, and will the patient maintain the same benefit?” Dr. Fleischmann asked.
Other long-term questions with tofacitinib relate to its safety profile, said Dr. Weinblatt. “We have two long-term observations with a small percentage having serious infections and some lab abnormalities that led to drug withdrawal,” he said. “This is an immunomodulating therapy, so seeing infections is not unexpected,” Dr. Weinblatt said. However, studies show that doses above 5 mg appear to be associated with more side effects, he said. This raises questions about differences in response and toxicity between tofacitinib 5 mg and 10 mg, he said.
There is also evidence of lipid elevation with tofacitinib use in some patients, he said.
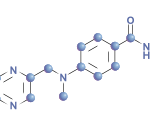
R788
Presenters also discussed fostamatinib disodium (R788, Rigel Pharmaceuticals), an oral inhibitor of Syk kinase. This drug is currently in phase III studies at twice a day dosing, Dr. Weinblatt said. Fostamatinib has been studied for treatment of lymphoma, lupus, and type 1 diabetes.
Research with fostamatinib in RA has shown efficacy with some side effects, such as loose stools or diarrhea in 20% of subjects and an increase in blood pressure in 25% of subjects in one study. “Twenty-five percent needed antihypertensive therapy or needed to increase their dose [of antihypertensive therapy],” he said. However, at the end of the study, subjects’ blood pressure was identical to baseline.
Dr. Fleischmann said the risk for hypertension is not strong as long as clinicians are aware of the risk and treat it appropriately.
Another question about fostamatinib that has yet to be answered is whether it is efficacious in the same population as tofacitinib, Dr. Fleischmann said.
Looking Ahead to Future Use
Ultimately, time will tell how kinase inhibitors will add to the treatment options for RA, the presenters said. “These agents can be used before methotrexate or another DMARD, after methotrexate or another DMARD, before a biologic, after failure of a tumor necrosis factor–1 [TNF-1] agent, after failure of a second TNF-1, or after failure of one or more other biologic,” Dr. Fleischmann said.
He discussed several possible scenarios for kinase inhibitors. If all studies show efficacy and the cost of these drugs is similar to currently available biologics, then he believes methotrexate will still be the first DMARD used. “It works in a third of patients, and it’s cheap,” he said. “The first agent after methotrexate would be a TNF-1 because of their long history of efficacy and known safety profile. Plus, there is no cost advantage to using the oral agents.”
If efficacy is found with kinase inhibitors but the cost of these agents is less than current biologics, Dr. Fleischmann said, methotrexate still will likely be the first DMARD used, followed by a kinase inhibitor and then a TNF inhibitor.
If new studies do not find that kinase inhibitors are as favorable as TNF-1 or other biologics and their cost is higher than what’s currently available, Dr. Fleischmann believes a treatment scenario of methotrexate followed by TNF-1s would be likely. “These agents would be the last ones used,” he said.
That said, Dr. Fleishmann predicted that the efficacy and safety of the kinase inhibitors will remain static with what research has found so far.
“I think, regardless of cost, most rheumatologists initially will use these medications in patients unresponsive to biologics,” Dr. Fleischmann said. “If they are successful, they will expand their use over time. Cost, patient preference, and comorbidities may lead to early adoption or avoidance.”
Vanessa Caceres is a freelance medical writer in Bradenton, Florida.