Rheumatologists help set the reimbursement rates for the services they provide—but only if they participate in the service valuation process that helps define reimbursement rates for specialty services.
Rheumatologists help set the reimbursement rates for the services they provide—but only if they participate in the service valuation process that helps define reimbursement rates for specialty services.
“It is so important for rheumatologists to understand the integral role they play in federal decisions for accurate reimbursement rates—starting with responding to AMA [American Medical Association] surveys when CPT codes that impact rheumatologic care come up for review,” stresses ACR Director of Practice Management Antanya Chung, MBA, CPC, CPC-I, CRHC, CCP.
Unfortunately, past member response to CPT valuation surveys has been extremely low. For example, when the last survey went out to 1,500 members in 2021 regarding services frequently submitted for rheumatology reimbursement, only 10 rheumatologists responded.
The AMA needs enough representative data from physician surveys to make accurate reimbursement recommendations to the Centers for Medicare & Medicaid Services (CMS). Otherwise, the determination of relative value units (RVUs) that drive reimbursement rates may not accurately reflect what rheumatologists actually spend to provide that care.
Ms. Chung works closely with Timothy Laing, MD, ACR representative to the AMA Relative Value Update Committee (RUC), and Gene Huffstutter, MD, ACR representative to the AMA Current Procedural Terminology (CPT) Code Committee, to advocate using members’ input for reimbursement that accurately reflects costs.
How the Relative Value Update Cycle Works
To help reiterate the roles members and the ACR play in the process to determine RVUs that inform CPT codes, Ms. Chung, Dr. Laing and Dr. Huffstutter share some quick highlights on key elements of the RUC/CPT cycle. With this knowledge, they hope members can be ready to participate in the process when they get a survey.
RUC/CPT cycle—In simple terms, Dr. Hufstutter explains the RUC/CPT process as follows: “CPT is how we are paid for our services. It describes the work we do as health providers. The RUC process values the work done. Both are essential to get adequate compensation for our services.”
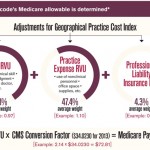
RVU value and CPT codes—The CMS has statutory authority to determine the values in the medical professional fee schedule. Each year, it sets a conversion factor that, when multiplied by the RVU value for each CPT code, determines the physician payment for that procedure, Dr. Laing explains. This conversion factor is currently estimated to be $32.7476 in the 2024 proposed rule.
AMA RUC Committee—All medical societies that meet the criteria for participation (for the ACR, 1,000 or more dues-paying AMA members) may participate in this committee, which serves in a voluntary advisory capacity to the CMS to recommend RVU values for both new and existing codes. As ACR’s representative on this committee, Dr. Laing attends committee meetings to share his input relevant to rheumatology.