Rheumatologists help set the reimbursement rates for the services they provide—but only if they participate in the service valuation process that helps define reimbursement rates for specialty services.
Rheumatologists help set the reimbursement rates for the services they provide—but only if they participate in the service valuation process that helps define reimbursement rates for specialty services.
“It is so important for rheumatologists to understand the integral role they play in federal decisions for accurate reimbursement rates—starting with responding to AMA [American Medical Association] surveys when CPT codes that impact rheumatologic care come up for review,” stresses ACR Director of Practice Management Antanya Chung, MBA, CPC, CPC-I, CRHC, CCP.
Unfortunately, past member response to CPT valuation surveys has been extremely low. For example, when the last survey went out to 1,500 members in 2021 regarding services frequently submitted for rheumatology reimbursement, only 10 rheumatologists responded.
The AMA needs enough representative data from physician surveys to make accurate reimbursement recommendations to the Centers for Medicare & Medicaid Services (CMS). Otherwise, the determination of relative value units (RVUs) that drive reimbursement rates may not accurately reflect what rheumatologists actually spend to provide that care.
Ms. Chung works closely with Timothy Laing, MD, ACR representative to the AMA Relative Value Update Committee (RUC), and Gene Huffstutter, MD, ACR representative to the AMA Current Procedural Terminology (CPT) Code Committee, to advocate using members’ input for reimbursement that accurately reflects costs.
How the Relative Value Update Cycle Works
To help reiterate the roles members and the ACR play in the process to determine RVUs that inform CPT codes, Ms. Chung, Dr. Laing and Dr. Huffstutter share some quick highlights on key elements of the RUC/CPT cycle. With this knowledge, they hope members can be ready to participate in the process when they get a survey.
RUC/CPT cycle—In simple terms, Dr. Hufstutter explains the RUC/CPT process as follows: “CPT is how we are paid for our services. It describes the work we do as health providers. The RUC process values the work done. Both are essential to get adequate compensation for our services.”
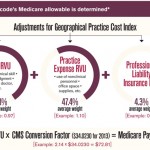
RVU value and CPT codes—The CMS has statutory authority to determine the values in the medical professional fee schedule. Each year, it sets a conversion factor that, when multiplied by the RVU value for each CPT code, determines the physician payment for that procedure, Dr. Laing explains. This conversion factor is currently estimated to be $32.7476 in the 2024 proposed rule.
AMA RUC Committee—All medical societies that meet the criteria for participation (for the ACR, 1,000 or more dues-paying AMA members) may participate in this committee, which serves in a voluntary advisory capacity to the CMS to recommend RVU values for both new and existing codes. As ACR’s representative on this committee, Dr. Laing attends committee meetings to share his input relevant to rheumatology.
“While participation does not guarantee a given RVU value request, absence from the committee process almost never produces a favorable result,” Dr. Laing says. “Aside from individual CPT code value determinations, the RUC also serves as a vital nexus of communication with other societies, the CMS and the AMA, allowing discussion of broader issues affecting all of medicine.”
CPT code review surveys—Surveys are sent out periodically to ACR members to demonstrate that survey responses truly represent the majority of practitioners’ work for a specific CPT code. Codes are not eligible for RUC valuation if the requisite number of surveys (the minimum threshold depends on national code utilization frequency) are not returned. The submitted responses form the basis for RUC committee debate, Dr. Laing shares.
When rheumatologists need to be surveyed, Ms. Chung coordinates with the AMA by suggesting ACR members who are likely to seek reimbursement for the CPT code up for review. Then a portion of ACR members who fall in this group are invited by email to answer the survey questions.
“This means that every ACR member who receives a RUC survey for a CPT code being considered for valuation or re-valuation should complete it to the best of their ability,” Ms. Chung stresses. She notes that survey language is very specific to reimbursement terminology, which can add to the challenge of answering the survey. She encourages any ACR member who receives a survey to contact the ACR with any questions, because their answer can make a significant difference in the final RVU determination.
Case in Point: CPT Code Review for Diagnostic Ultrasound
Starting in 2021, ACR members were surveyed for several code re-valuations, including for diagnostic ultrasound CPT codes 76881 and 76882. The goal was to present practice expenses for this code, because there were questions about the utilization of the codes and what was being done in practice, Ms. Chung explains. “ACR members became key players in this code set because rheumatology is the largest specialty that uses these codes, representing 25% of Medicare claims data.”
Between 2021 and 2023, Ms. Chung, Dr. Laing and Dr. Huffstutter worked with other physician specialties to communicate to the AMA and, thereby, the CMS on what was required in practice for these codes, spanning from the actual equipment purchasing and maintenance costs to clinician time spent collecting and analyzing ultrasound data for diagnosis.
“We proved these codes and the care they represent are very important to managing care for patients with rheumatic disease, as well as other patients in pain,” Ms. Chung says. For the final RVU determination, CPT code 76881 decreased, but CPT code 76882 increased. “In the big scheme of things, our success with securing an RVU increase for one of these diagnostic ultrasound codes gives us an idea of the advocacy work we can do to make changes in the future.”
She stresses the added value members can play in this advocacy by responding to future surveys to provide as much physician input as possible to help the CMS make the right decisions on care costs and reimbursement to allow practices to recoup those costs.
Reimbursement Developments in the Coming Year
Looking ahead to 2024, Ms. Chung expects that CPT codes used in rheumatology could come up for review, and she wants members to be ready. Here’s what members can expect if this happens:
- As soon as the ACR learns a CPT code review could impact members, the College will communicate this information broadly through news and social media channels. Here’s an example sent in 2019.
- Next, members should be ready to receive a survey via email, keeping in mind that only 1,500 or so members will get the survey. A blank survey illustrates what it looks like.
- Find detailed instructions for how to navigate the survey.
Dr. Laing encourages all ACR members to keep an eye out for news and social media posts specific to any topics related to payer activity, because the ACR advocates on behalf of rheumatology at the federal level on many important payment issues. For example, this year Ms. Chung participated in edits to evaluation and management documentation guidelines designed to support decision making in determining which code to bill. “Antanya Chung has extensive knowledge of the complex landscape of payment practices, and she has more than 20 years of experience working directly with payers and those who advocate appropriate payment for rheumatology services,” Dr. Laing notes.
Ms. Chung stresses the value of members sharing their payment experiences with the ACR, because “this direct awareness of what physicians are experiencing in practice is often the catalyst for the ACR to share their concerns with those making payment decisions.”
ACR members can communicate any questions regarding payment concerns or questions about reimbursement, coding and the RUC/CPT survey process by contacting Antanya Chung directly at [email protected] or (404) 633-3777 x818.
Carina Stanton is a freelance science journalist based in Denver.