A practice receives an overpayment request from the Centers for Medicare & Medicaid Services (CMS) for not meeting medical necessity related to a biologic infusion. In which instructional guideline can the coding and billing staff find the necessary information on the CMS website to handle this request? Internet-only manuals National Correct Coding Initiative Medically Unlikely…
Articles by From the College
How to Navigate & Manage Insurance Overpayments
Insurance overpayments can occur in a practice for a variety of reasons. An insurer may simply make a mistake by paying a provider more than the contracted amount for a service or pay for a service that is not covered under the patient’s insurance plan. Whatever the reason, overpayments can and will create headaches for…
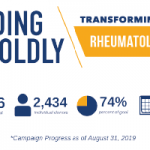
Leading Boldly: Transforming Rheumatology Campaign Makes Progress
In 2018, the Rheumatology Research Foundation embarked on its third and most ambitious fundraising campaign, Leading Boldly: Transforming Rheumatology, with a goal of raising $75 million over five years. The campaign supports Foundation programs to recruit the best and brightest into the field, train rheumatology professionals at all career stages and support investigators conducting research…
Check Out the Wellness Pavilion at the 2019 ACR/ARP Annual Meeting
With massage chairs, creative spaces and therapy dogs, the Wellness Pavilion will offer this year’s Annual Meeting attendees respite from the busy conference atmosphere…
Coding Corner Answer: An Insurance Billing Quiz
Take the challenge. A—The commercial insurance coverage is primary in this situation. Medicare should be billed secondarily because it will not become primary until after the first 30 months of ESRD Medicare entitlement. After that, Medicare will be primary no matter the patient’s employment status. C—Unless the patient has a qualifying condition, such as ESRD,…
Coding Corner Question: An Insurance Billing Quiz
A 55-year-old male patient diagnosed with generalized osteoarthritis and diagnosed with end stage renal failure (ESRD) 20 months previously presents to the office to see the rheumatologist. The patient has a commercial insurance plan and Medicare. Which carrier is primary for this visit? Commercial insurance carrier Medicare You do not know because it is not…
Pediatric Rheumatology Learning at the 2019 ACR/ARP Annual Meeting
At this year’s ACR/ARP Annual Meeting, Nov. 8–13, all of the pediatric rheumatology sessions will take place in the same room, making it easy to access all of the exciting content. Planners hope this convenient setup facilitates networking before and after symposia. “In pediatric rheumatology, we are very tight-knit community. This [event] is our opportunity…

Annual Meeting Preview: Rheumatology Research Foundation Activities
Another exciting ACR/ARP Annual Meeting is planned for this November. Show your support for the Foundation’s mission and enjoy your time in vibrant Atlanta at one of the Foundation’s events. Donations made to the Foundation support the extensive awards program that funds research, training and education opportunities for current and potential rheumatologists and rheumatology professionals…
ACR Leads Coalition Opposing Cigna’s Elimination of Consultation Codes
In a letter co-signed by other Cognitive Specialty Coalition organizations, the ACR is requesting at least a one-year delay to better coordinate payer changes with recent federal initiatives.
UnitedHealthcare Delays Policy Changes Affecting Physician-Administered Treatments
Changes announced at the beginning of October have now been delayed for Actemra, Benlysta, Cimzia, Orencia and Simponi Aria, but changes to the Stelara policy remain in effect.
- « Previous Page
- 1
- …
- 29
- 30
- 31
- 32
- 33
- …
- 94
- Next Page »