On Feb. 1, UnitedHealthcare enacted a new policy designating Avsola and Inflectra as the preferred infliximab products for UHC commercial plans. ACR leaders have urged UHC to allow existing patients to continue on their current medication.

A New Era of Coding Evaluation & Management Services
After 25 years, the American Medical Association (AMA) Current Procedural Terminology (CPT) office and outpatient evaluation and management (E/M) codes received a major overhaul. These changes, which went into effect Jan. 1, will help reduce administrative burden on providers and roll back some of the rigid requirements for E/M coding by simplifying the code selection…
Evaluation & Management Coding Changes in the 2021 Physician Fee Schedule Final Rule
Implementation of rate increases for evaluation and management services and other changes bring big updates to many Current Procedural Terminology codes.
UHC Updates Rituximab Policy to Require Use of Biosimilars
As of Oct. 1, UnitedHealthcare (UHC) requires that patients fail to respond to both FDA-approved rituximab biosimilars prior to receiving approval for rituximab. Exception: Rituximab-pvvr (Ruxience) is not FDA approved for rheumatoid arthritis.
ACR Convergence 2020 Workshop Covers 2021 Practice Management & Coding Changes
Attendees at the daylong workshop will learn about key evaluation and management code changes coming in 2021 that affect rheumatologists and rheumatology professionals.
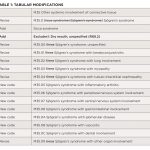
Changes in ICD-10 for Sjögren’s Syndrome
A code change in the ICD-10 classification for Sjögren’s syndrome was approved by the ICD-10 Coordination and Maintenance Committee in July 2019 and becomes effective October 2020.

Best Practices for COVID-19 Regulatory Waivers, Relief Funding & Audits
When the first laboratory-confirmed COVID-19 case was reported by the Centers for Disease Control & Prevention (CDC) on Jan. 22, it was difficult to predict an ensuing global pandemic would last for more than half the year. Approximately one week after the initial CDC report, the U.S. Department of Health & Human Services (HHS) declared…
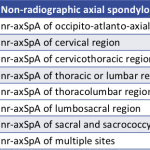
Non-Radiographic Axial Spondyloarthritis Recognized with ICD-10 Code
The new diagnostic code should streamline billing for treatment of nr-axSpA, better define the spectrum of spondyloarthritic diseases and enable new research strategies into these conditions.
Locum Tenens as a Resource for Practices During the COVID-19 Outbreak
As the number of COVID-19 cases continues to rise in the U.S., the fast spread of the virus is causing gaps in practice staffing, and patient influx will likely increase, leaving systems needing more providers. The use of locum tenens physicians can help practice fill gaps at your organization caused by COVID-19. Below we offer…

Reimbursement Tips: Telemedicine & Coding in the Time of COVID-19
Humans may fear change as a general rule, but we’re adaptable when we need to be. In this era of COVID-19 and social distancing, medical practices and payers are adapting to an increased use of telemedicine, which enables providers to see their patients without being in a room with them. To cope, the Centers for…
- « Previous Page
- 1
- …
- 3
- 4
- 5
- 6
- 7
- …
- 55
- Next Page »