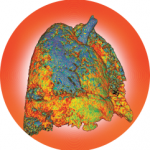
SAN FRANCISCO—The 13th International Congress on Systemic Lupus Erythematosus (SLE), held April 5–8, highlighted continuing advances in the fight against lupus, a chronic, inflammatory, autoimmune disease affecting multiple organ systems. The rheumatologist’s ability to control this incurable and life-threatening condition is limited both by its heterogeneous presentation and by the lack of successful treatment options,…