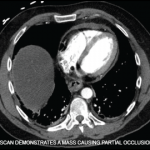
Defined by the presence of antiphospholipid antibodies (aPL) in individuals with clinical evidence of thrombosis or pregnancy morbidity, antiphospholipid syndrome (APS) is a systemic autoimmune thrombophilia. Clinical thrombosis, which should be confirmed by objective validated criteria (e.g., imaging studies or histopathology), can occur in the arterial, venous or small vessel vasculature and is not limited…