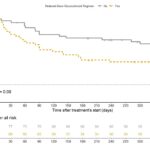
Background/Purpose Polymyalgia rheumatica (PMR) treatment is primarily based on long-term corticosteroids, which results in significant toxicities. Studies have shown that patients with PMR are exposed to years of corticosteroid treatment.1,2 In a single academic center cohort, we found that 76% of patients remained on steroids at the end of two years.3 In a second cohort…