Review 28 recommendations covering proteinuria screening, biopsy indications & triple therapy regimens for lupus nephritis.
Why Target B Cells in SSc-ILD?
In a recent Arthritis & Rheumatology review article, three experts discuss the use of immunosuppressants to target B cells in a patient with systemic sclerosis-interstitial lung disease.

Rheumatology Medications with Limited Safety Data: How Do We Use Them in Pregnant Patients?
How does a rheumatologist treat a pregnant woman when many medications are not approved for pregnancy or safety data are limited?

Lessons Learned from Two Scleroderma Lung Studies (Plus a Third That’s Recruiting Sites)
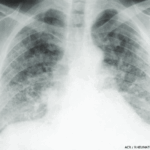
Historically, the early approach for treating interstitial lung disease (ILD) due to systemic sclerosis (SSc) involved immunosuppressant therapy, primarily with cytotoxic agents.1 Glucocorticoids in combination with another immunosuppressant agent, such as oral azathioprine or cyclophosphamide, were often used to treat patients with severe, progressive SSc-ILD.2 However, direct evidence to support this therapeutic approach was lacking…

Treatment Tips for Pulmonary Arterial Hypertension & ILD
CHICAGO—About 30 years ago, pulmonary arterial hypertension (PAH) and interstitial lung disease (ILD) began to outpace renal crisis as the main causes of death in scleroderma (SSc). But treating these lung complications has proved vexing for clinicians. There is no easy way to predict who will develop PAH. There is no telltale antibody and no…

Infection Rates for Patients with SLE on Immunosuppressive Drugs
A comparison study of the serious infection burden among patients with lupus found no major differences in patients treated with three separate immunosuppressive drug regimens. Given that serious infections are among the leading causes of hospitalizations and death in patients with systemic lupus erythematosus (SLE), researchers investigated whether the incident rates differed in patients who…

From the Expert: New Advances in Treatment of Systemic Scleroderma
A recent study found that mycophenolate mofetil is an effective alternative for the treatment of systemic scleroderma with interstitial lung disease, resulting in possible long-term improvement. According to Aryeh Fischer, MD, this new research points to the future expansion of treatment options…

Lupus Nephritis Therapies Compared, Plus Naming Guidance for Biosimilars
Comparing tacrolimus, mycophenolate mofetil and cyclophosphamide, tacrolimus was the most efficacious. Also, biosimilars may soon be easier to differentiate…
Best Lupus Treatment Still Up for Debate
Panel looks at decision making for treatment of three high-risk patients
Drug Updates
Information on New Approvals and Medication Safety