Shidlovski/shutterstock.com
CHICAGO—Caryn A. Libbey, MD, clinical associate professor of medicine at Boston University School of Medicine, described the evolving in our understanding of amyloid at the ACR’s State-of-the-Art Clinical Symposium in April. Amyloidosis is a rare disease that is often underdiagnosed and undertreated.
“Even though this disease has been around for 150 years, I still consider it a relatively modern disease, because the first fibril was identified only in 1971,” explained Dr. Libbey. There are more than 30 amyloid precursor proteins, which, in healthy individuals, remain soluble. When proteins, such as the kappa or lambda light chain or transthyretin, become insoluble, they can cause amyloidosis.
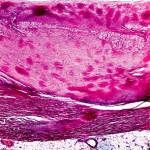
The insoluble molecules can be visualized in the tissue as nonbranching beta pleated sheets that stain positive for Congo red. Unless the stain is performed properly, there may be a 10–15% false-positive rate and a 10–15% false-negative rate. Unfortunately, the stain is infrequently performed because pathologists do not often have amyloidosis as a differential diagnosis unless the clinician has alerted the pathologist. Diagnosis of amyloid is made only when a biopsy is positive.
Types of Amyloid
Local amyloid—This type may form without systemic deposition in skin, the larynx/bronchus or bladder, or less often, the breast or lung.
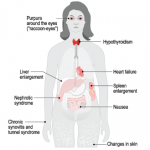
AL (amyloid from light chain)—AL patients frequently experience malaise, weight loss and fatigue. They often have proteinuria with or without decreased glomerular filtration rate. Approximately 45% of patients with amyloidosis have cardiac symptoms that present as congestive heart failure, restrictive cardiomyopathy, edema, arrhythmia and/or heart block. In addition, approximately one-third of patients have neuropathy that presents in peripheral sensory and motor nerves or in autonomic nerves. Foot pain is especially common in these individuals, for which a patient may be referred to rheumatology.
AA (amyloid from serum amyloid A deposition)—Amyloid A (AA) amyloidosis is more likely to be seen by rheumatologists outside the U.S. It is caused by chronic uncontrolled inflammation and can result from tuberculosis, osteomyelitis, rheumatoid arthritis, ankylosing spondylitis, Crohn’s disease, juvenile idiopathic arthritis and psoriatic arthritis, among other causes (see sidebar below).
ATTRm (amyloid from point mutation of transthyretin)—Most rheumatologists won’t encounter transthyretin-related neuropathic amyloidoses (ATTRm), rare, familial forms of amyloidosis first described in 1952. Most often, ATTRm presents with neuropathy, cardiomyopathy and nephropathy.
More than 120 point mutations have been described that result in familial ATTR, but some mutations are more common than others. A Portuguese mutation has a high penetrance, and thus, most individuals who inherit the gene will express symptoms of disease. The age of onset of individuals with the Portuguese mutation is 25–30 years. These individuals experience progressive peripheral sensorimotor neuropathy, followed by cardiac and renal symptoms. The patient often dies within 10 years of diagnosis, if untreated.