There are two “new” diseases of the late 20th century—AIDS and the antiphospholipid syndrome.
—Miguel Villardel, MD, professor of medicine, Hospital Valle de Hebron, Barcelona
Since its clinical description in 1983, antiphospholipid syndrome (APS or Hughes Syndrome) has become the domain not only of rheumatologists and obstetricians, but of neurologists, cardiologists, psychiatrists, otolaryngologists, and orthopedists. Like lupus, APS embraces all clinical specialities.
Brief History of APS
In 1983, my colleagues and I described in detail a syndrome involving—uniquely—both arterial and venous thrombosis, and including prominent neurological features, including strokes, seizures, memory loss, and chorea. In addition, this syndrome was associated with occasional thrombocytopenia, livedo reticularis, labile hypertension, recurrent miscarriage, and internal organ thrombosis such as Budd-Chiari syndrome.1,2 We recognized that the syndrome was “sufficiently different from typical systemic lupus to warrant separate consideration”—originally calling it the anticardiolipin syndrome.2 Led by the late Aziz Gharavi, MD, and E. Nigel Harris, MPhil, MD, DM, we set up sensitive immunoassays for antiphospholipid antibodies (aPL), changed the name to APS, and introduced the term primary APS for stand-alone cases.2,3
The worldwide interest in this syndrome has led to its recognition in a wide variety of clinical states increasing diagnosis. Indeed, it seems a fairly safe prediction that APS will overtake lupus in prevalence. A rough one-in-five rule seems to apply for the contribution of APS to various clinical conditions—one in five cases of recurrent miscarriage, one in five strokes in people under 45, one in five cases of deep vein thrombosis (DVT). Eventually, this estimate may also pertain to other major illnesses including myocardial infarction in the young, idiopathic teenage epilepsy, and possibly even migraine.
Pathogenesis and Clinical Features
APS is an autoimmune disease in which antibodies directed against phospholipid-protein complexes appear to lead directly to thrombosis. Like all autoimmune diseases APS has a genetic component, and cases of thyroid disease, Sjögren’s syndrome, and lupus are frequently seen in families with APS.
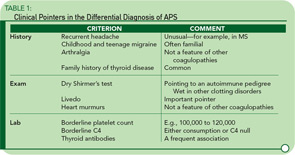
While arterial and venous thromboses are the hallmarks of the syndrome, there are other clinical clues. Headache—particularly migraine—is often an early feature going back to childhood, and often familial. Livedo reticularis is an important physical sign, and a dry Shirmer’s test, suggesting underlying Sjögren’s syndrome, is a clue to the disease’s autoimmune pedigree. Table 1 lists some of the major differences between APS and other pro-thrombotic disorders.
Neurological Considerations
Stroke: The most feared complication of APS is stroke, with up to 20% of strokes in people under 45 possibly having this etiology. In this setting, the MRI can be misleading (e.g., false negatives) and we look forward to the development of more sensitive and available screening techniques. Estimates for the frequency of stroke in patients with APS vary widely, and some studies have been hampered by methodological problems.4