BACK SURGERY
Long-term Outcome of Herniated Disc Surgery
By David G. Borenstein, MD
Abstract
Study design: A retrospective, follow-up cohort study.
Objective: To evaluate the 25-year (or longer) outcome of discectomy for lumbar disc herniations by validated instruments.
Summary of background data: A comprehensive patient-oriented evaluation should include measurements of pain and disability along with a reliable evaluation of the general health status. There is a paucity of data from validated measuring instruments on the very long-term outcome of lumbar discectomy.
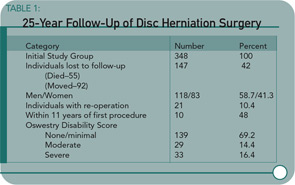
Methods: The authors conducted a follow-up study of 201 patients an average of 27.8 years (range 25-32) after lumbar discectomy. The patient-oriented assessment included a Short Form-36 Health Survey questionnaire, Oswestry Disability Index, Cumulative Illness Rating Scale, and a study specific questionnaire dealing with daily life activities and satisfaction with the surgery.
Results: The Short Form-36 Health Survey physical scales and summary scores were similar to the normative values for healthy subjects and were better than the scores of patients with untreated sciatica with respect to reported pain. The mean Oswestry disability score was 17.5. Satisfaction with surgery was expressed by 181 of 201 patients (90%).
Conclusions: Patients who had undergone lumbar discectomy a minimum of 25 years earlier have a satisfactory self-reported health-related quality of life and less pain than non-surgically treated subjects.
Commentary
An important concern for patients with radiculopathy associated with intervertebral disc herniation involves the better short-term and long-term outcomes associated with surgical discectomy versus medical therapy. Patients need to balance the possibility of rapid resolution of back and leg pain against the potential risks of advanced spinal degeneration caused by surgical intervention. Prior studies have reported a benefit for surgical patients early in the post-operative period. In a prospective study of 126 patients randomized to surgical discectomy versus conservative therapy, the difference in early surgical benefits tends to equalize over a 10-year follow-up period as reported by Weber.1 However, the effects of surgery on clinical symptoms and advancement of spinal degeneration over a longer period than a decade were unknown.
I was reassured by the overall results of this long-term, 25-year follow-up study reported by Mariconda and colleagues demonstrating the satisfaction of surgical patients with their operations as documented by validated outcome measures. A majority of patients undergoing surgery can be pain-free and functional without progressive spinal disorders. I was concerned, however, about several aspects of the study. For example, a significant number of individuals from the initial cohort have been lost to follow-up. Also, a small but significant proportion of study enrollees required additional spinal surgeries and were disabled.