A 56-year-old automobile mechanic was referred to our rheumatology service by his orthopedist to evaluate left posterior knee pain and swelling that had been present for three months. The patient had undergone bilateral total knee arthroplasties (TKAs) for sports-related osteoarthritis three years before.
In addition to the knee pain, the patient described several years of bilateral hand swelling and stiffness, which had been worsening over the past few months. He also complained of significant malaise and fatigue over the past six months. He denied a history of spine pain or stiffness, psoriasis or bowel problems.
Physical examination revealed chronic synovitis of the bilateral wrists and metacarpophalangeal (MCP) joints and a swelling posterior to the left knee. There was no clinical or X-ray evidence of arthroplasty failure or loosening. Review of the surgical report revealed no posterior left knee mass or bursal enlargement.
Ultrasound of the left knee demonstrated a cystic mass superficial to the tendons of the medial gastrocnemius and the semimembranosus muscles measuring 1.63 cm in depth and 6 cm in length. The cyst consisted of a mixture of hyper- and hypoechoic areas and a smaller relatively anechoic area. Power Doppler was negative. Careful inspection did not demonstrate a stalk connecting the mass to the arthroplasty (see Figures 1 & 2).
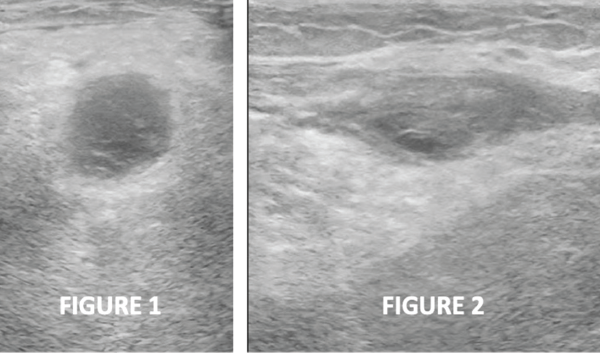
Figures 1 & 2: Transverse and longitudinal ultrasound views, respectively, of the left posterior knee, revealing a cystic mass with heterogeneous internal echotexture and no stalk.
Ultrasound of the left hand confirmed the clinical finding of significant chronic synovitis, as noted by an enlarged dorsal synovial recess filled with hyperechoic material, as well as severe bony and cartilaginous erosion of the second and third MCP joints. Osteophyte formation was noted as well (see Figure 3). Power Doppler was only minimally positive. Left hand X-rays (see Figure 4) corroborated severe MCP narrowing and osteophytes at MCP joints 2 and 3, with mild osteoarthritic change at the proximal phalangeal joints. Opposite hand X-rays demonstrated periarticular cortical erosions of MCP joints 2 and 3. Neither ultrasound nor the X-rays suggested calcium deposition in soft tissues.
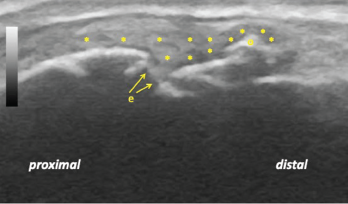
Figure 3: Longitudinal ultrasound view of the left second metacarpophalangeal joint demonstrating diffuse synovitis (*), metacarpal head discontinuity due to bone and cartilage erosion (e), and a bony osteophyte (o).
Anti-nuclear antibody, anti-cyclic citrullinated peptide antibody, rheumatoid factor, serum calcium, angiotensin converting enzyme, Lyme serology, uric acid level, iron studies and a chest X-ray were negative or unremarkable. His erythrocyte sedimentation rate was normal at 15 mm/hour.
The patient declined cyst aspiration. With a working diagnosis of seronegative rheumatoid arthritis (RA), methotrexate (MTX) was prescribed. Weekly MTX administration of 20 mg subcutaneously effected substantial improvement of pain and swelling, but only mild improvement of hand stiffness. Fifty milligrams of subcutaneous etanercept weekly was ordered to improve joint stiffness and fatigue.



