About time / shutterstock.com
ATLANTA—The potential of cannabis‐based medicines is a hot topic, particularly as pain management therapy for arthritis and other conditions. However, confusion abounds regarding its therapeutic potential, how it can be administered and even the correct terminology to use.
David P. Finn, PhD, professor of pharmacology and therapeutics, and founding co-director of the Centre for Pain Research at the National University of Ireland, Galway, spoke at the 2019 ACR/ARP Annual Meeting in the session, Mechanisms of Cannabinoids in Pain Management. He discussed the potential for this controversial plant and its derivatives.
Although the cannabis plant has three species, Cannabis sativa is the one that has the most interest and potential medicinally, Dr. Finn pointed out.
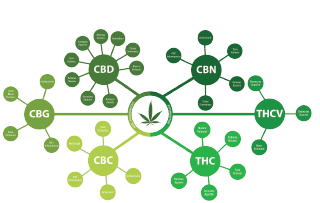
“When talking about cannabinoids, we’re talking about biologically active constituents of cannabis (phytocannabinoids) or synthetic compounds, usually having affinity for and activity at cannabinoid receptors,” said Dr. Finn. As many as 1,000 unique molecules are contained in the cannabis plant. To date, cannabis plants and plant material, including flowers, hashish, buds, leaves and full plant extracts, have been used for medical reasons.
Cannabis-based medicines also exist. These are registered as medicinal cannabis extracts with defined, standardized tetrahydrocannabinol (THC) and cannabidiol (CBD) content. These are classified as cannabis-derived or cannabis-based medicines. Examples: 1) nabiximols (Sativex), a cannabis-based pharmaceutical product containing delta 9-THC and CBD in a 1:1 ratio, delivered in an oromucosal (mouth) spray; it has been approved as adjunctive treatment for neuropathic pain in patients with multiple sclerosis; and 2) Epidiolex, an oral CBD solution used to treat seizures caused by two forms of epilepsy: Lennox-Gastaut syndrome and Dravet syndrome.1
Molecular Targets
Many years after THC was discovered, the molecular targets mediating its effects were identified—the cannabinoid receptors CB1 and CB2 and their endogenous ligands. The endocannabinoid system is the regulatory system in the body that controls the creation and breakdown of cannabinoids. It also plays a key role in mediating pain sensation, appetite, sleep and metabolism.

Dr. Finn
CB1 is associated with psychoactive, neuromodulating and analgesic effects due to the THC lipid. CB1 is ubiquitously distributed and expressed across the entire body, in the brain, adipocytes, hepatocytes and musculoskeletal tissues. “Based on studies, CB1 is the most highly expressed G-protein-coupled receptor in the brain,” said Dr. Finn.
CB2 is associated with anti-inflammatory and immunomodulatory effects but has no psychoactive effects. CB2 is expressed in body cells controlling immune function and, possibly, the central nervous system.
As described in the European Pain Federation (EFIC) position paper, Appropriate Use of Cannabis‐Based Medicines and Medical Cannabis for Chronic Pain Management, the lipid signaling system of the endocannabinoid system plays a very important role in the regulation of a wide array of physiological processes, including appetite, metabolism, mood, motor function, gastrointestinal tract function, cardiovascular control, stress response, developmental biology, cell fate, immune and inflammatory response, endocrine function, neurotransmission and pain.2
Efficacy Studies
Many studies have focused on the efficacy of cannabinoids in chronic pain, the most common condition cited by patients for the medical use of cannabis, according to Dr. Finn. A report released by Ireland’s Health Products Regulatory Authority in 2017 stated, “chronic pain is the most studied indication for cannabinoids.”3



