Myelofibrosis is a hematologic process characterized by bone marrow reticulin fibrosis and mainly associated with myelodysplastic disorders in which the level of fibrosis is variable. It can also present in the setting of an autoimmune disease, hence the term autoimmune myelofibrosis (AMF).
AMF is a rare condition that has been linked to systemic lupus erythematosus (SLE). For example, in one series of 27 patients with AMF, 18 had SLE.1 However, there are only two prior cases of AMF affecting Hispanic patients with SLE reported in the medical literature.2
Case report
Our patient is a 25-year-old Hispanic female with SLE characterized by myositis, nephrotic syndrome and cutaneous lesions. Laboratory abnormalities included a positive antinuclear antibody (ANA), anti-Smith antibodies, double-stranded DNA antibodies, autoimmune hemolytic anemia, proteinuria, hypocomplementemia and elevated liver enzymes. The latter were thought to be consistent with autoimmune hepatitis (AIH).
In 2005, she was admitted with pancytopenia (total leukocyte count 3,000/mm3, differential: neutrophils 89%; lymphocytes 7%; monocytes 4%; hemoglobin 8.3 g/dL; hematocrit 24%; platelet count 10/mm3). She was initially treated with methylprednisolone at 1 mg/kg a day and mycophenolate mofetil 500 mg twice a day without improvement in her cell counts.
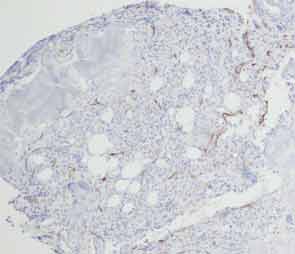
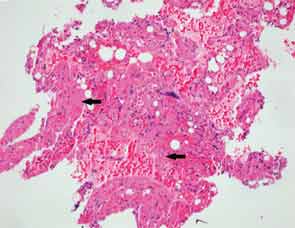
A bone marrow biopsy showed the presence of myelofibrosis with decreased hematopoietic cells on CD34 immunohistochemical stain and replacement of normal bone marrow with fibrotic tissue (see Figures 1, cover, and 2). The patient was pulsed with high-dose IV methylprednisolone and a five-day course of intravenous immunoglobulin (IVIG). Her cell counts improved with a leukocyte count of 7,500/mm3 (differential: neutrophils 81%; lymphocytes 8%; monocytes 11%); hemoglobin 8.6 g/dL; hematocrit 25%; and platelets 104,000/mm3.
An attempt was made to decrease her dose of corticosteroids by instituting a regimen of mycophenolate mofetil and tacrolimus. However, the patient developed new leukopenia episodes when the steroid dose was decreased. She was evaluated for a new episode of neutropenia, thought to be caused by her immunosuppressant medications because it improved after these drugs were stopped. She was later restarted on tacrolimus 2 mg BID, and azathioprine was added to treat the AIH (liver enzymes: AST 99; ALT 133; leukocyte count 4,000/mm3; hemoglobin 10.1 g/dL; hematocrit 29%; platelet count 136/mm3).
The patient moved to Mexico (2008–2012) and was managed only with prednisone 10 mg daily. When the patient was seen after a hiatus of four years, she was restarted on azathioprine 100 mg daily. This was increased to 150 mg when her liver enzymes increased following a decrease in her prednisone dose. Unfortunately, she developed pancreatitis that was attributed to the azathioprine, and it was discontinued. The prednisone dose was increased to 60 mg daily and slowly tapered to 15 mg per day. However, her liver enzymes rose again, and she was given a trial of mycophenolate mofetil 1 g BID. She presented with a new episode of pancytopenia, and this medication was discontinued.
