BOSTON—The uncertainty that surrounds the diagnosis of primary angiitis of the central nervous system (PACNS) is “as great as, if not greater than, the diagnostic uncertainty for any other disease encountered in rheumatology,” Leonard H. Calabrese, DO, said at a presentation at the ACR/ARHP Annual Meeting in Boston in November 2014. Diagnostic failure—failure to either recognize the disease or to correctly label a mimic of the condition—is unfortunately common, he said.
Speaking at the session, Primary Angiitis of the Central Nervous System and Its Mimics, Dr. Calabrese outlined the many reasons why diagnosis is difficult. “It is a rare disease, there are no good animal models, we have no high-efficiency investigation that is noninvasive that can readily make this diagnosis, and we are stimulated by the fact that we do need the diagnostic outcome to be favorable.”
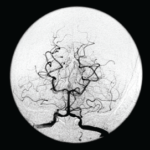
Clinicians seeking a diagnosis may apply the wrong test or rely on vascular imaging when the disease involves a vessel too small for spatial resolution to identify. “More commonly, the errors [of diagnosis] are cognitive,” said Dr. Calabrese, professor of medicine at Cleveland Clinic Lerner College of Medicine.
A brain biopsy has positive predictive value to rule in the diagnosis of PACNS.
Working criteria, proposed by Drs. Calabrese and Mallek in 1988, outlined the three conditions that must be met for a diagnosis: unexplained neurologic deficits, such as headaches, seizures, multiple strokes, cognitive dysfunction or visual problems, that remain unexplained after a neurologic workup; angiographic features that are compatible with PACNS or a positive biopsy of CNS tissue; and thorough exclusion of all the conditions that could mimic the angiographic finding or could produce a similar pathology, such as infection or malignancy.1 Identifying the mimics is “extraordinarily important” for an accurate diagnosis; some are quite common and some are rare, he said.2
Diagnosis Requires a Team
“There is no specialist or clinician who is an expert in all of the mimics; thus, one of the best practices in approaching CNS vasculitis is to make the diagnosis in a center where there are multiple interested individuals who have multiple skill sets,” he said. Most importantly, diagnosis should never be made based on any single diagnostic activity.
A diagnosis of PACNS should be seriously considered as a possible diagnosis when the patient has chronic meningitis with an aseptic formula for about a six-week period; multiple strokes in multiple vascular territories distributing over time; and focal signs from multiple strokes in different territories, as well as diffuse neurologic dysfunction.