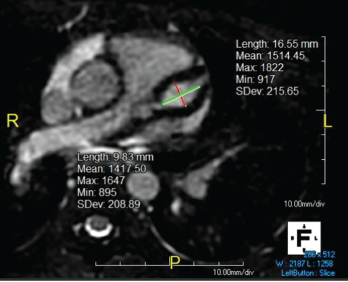
Figure 1. Giant LAD fusiform aneurysm measuring 9.8 mm in diameter (z-score = 19) and extending approximately 17 mm.
In September 2019, a previously healthy, 9-year-old white girl presented to the emergency department following two months of sinusitis and unexplained fever responsive to ibuprofen. She presented with anorexia; a 9 lb. weight loss; intermittent, nonbilious, nonbloody emesis; and occasional epistaxis with digital manipulation of the nose.
Six weeks prior to admission, she had presented to the emergency department with fever and rhinorrhea unresolved by amoxicillin. An evaluation revealed an erythrocyte sedimentation rate (ESR) of 58 mm/hr (reference range [RR] 0–20 mm/hr), a C-reactive protein (CRP) level of 22 mg/L (RR: 0–9 mg/L), a white blood cell (WBC) count of 17.6 cells/μL (RR: 5.4–9.7 cells/μL) and a hematocrit level of 41% (RR: 35–43%). A chest radiograph was unrevealing, and the urinalysis was normal, demonstrating a baseline creatinine (Cr) level of 0.4 mg/dL (RR: 0.31–0.61 mg/dl). She tested positive for enterovirus and was sent home with conservative management.
Two weeks prior to admission, the patient had been seen by an infectious disease specialist due to persistent fevers. Lactate dehydrogenase (LDH), uric acid, cytomegalovirus and Epstein-Barr virus titers were performed and found to be normal. She was noted to be incompletely vaccinated.
On admission, a physical examination revealed pale, friable nasal mucosa; a subtle transverse nasal crease; livedo reticularis on her hands and feet; and pseudofolliculitis in the lower extremities. She had no maxillary tenderness, and pulmonary and cardiac exams were unremarkable. Her vital signs were within normal limits.
Laboratory testing on admission showed an ESR of 10 mm/hr, a CRP of 16.3 mg/L, a WBC of 22.0 cells/μL, hematocrit of 26%, platelets of 574 K/uL (RR: 150–400 K/uL), Cr of 1.3 mg/dL and lactate dehydrogenase (LDH) of 944 U/L (RR: 420–750 U/L). Urinalysis revealed 10–25 RBC/HPF (normal: <5) and 5–10 WBCs/HPF (normal: <5/HPF), but was negative for protein and leukocyte esterase.
The patient was admitted for pre-renal azotemia, leukocytosis and fever of unknown origin, and intravenous ceftriaxone and fluids were administered.
As part of the evaluation for a fever of unknown origin, an echocardiogram was performed and revealed severe bilateral fusiform aneurysms 6–7 mm in diameter in both coronary arteries, as well as mild tricuspid, mitral and aortic valve regurgitation. An electrocardiogram showed 1 mm ST depressions in the lateral leads and QT prolongation to 541 ms. Troponin was initially 0.09 ng/mL (RR: 0–0.08 ng/mL), but normalized at 12 hours.
An abdominal ultrasound showed loss of corticomedullary differentiation in both kidneys. Magnetic resonance angiography (MRA) revealed a wedge-shaped region of enhancement suspicious for subacute to chronic renal infarct. MRAs of the chest, abdomen and head showed no other aneurysms.
Her hematocrit dropped to 24%. The patient’s valvular involvement was atypical for Kawasaki disease, and additional laboratory tests demonstrated proteinase-3 IgG >8.0 U (<0.4 U), C-ANCA (anti-neutrophil cytoplasmic antibodies) 1:256 (negative), anti-nuclear antibodies (ANA) 1:320 (normal: <1:40) with a speckled pattern, and normal complement levels. It was not until 10 days later that her urinalysis indicated proteinuria and a urine protein to creatinine ratio of 3.4.