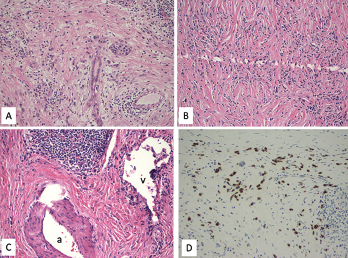
Figure 1. A. Lymphoplasmacytic infiltrate with pancreatic exocrine component atrophy. There is a cluster of remaining islet cells in the pancreatic duct. H&E magnification x200; B. Dense fibrosis with storiform pattern. H&E magnification x200; C. Lymphoplasmacytic infiltrate of a vein (phlebitis) without obliteration of the lumen. H&E magnification x200; v—vein, a—artery; D. Immunostain for IgG4 highlights increased IgG4-positive plasma cells, up to 80 cells/HPF. Immunostain, magnification x200.
Sarcoidosis and IgG4-related disease (IgG4-RD) are both immune-mediated, often multi-organ, diseases of uncertain etiology capable of presenting with diverse clinical manifestations. Many clinical features are common to both conditions, including hypergammaglobulinemia, the ability to form inflammatory masses and involvement of the lymph nodes, lacrimal glands, salivary glands, meninges and lungs. Although imaging modalities, such as positron emission tomography/computed tomography (PET/CT), and serologic evaluation may suggest one disease over the other, these diagnoses remain dependent on tissue sampling and histopathologic examination. Histopathologic evaluation is also essential to rule out other mimicking conditions, such as lymphoma.
Here, we present the case of a patient previously diagnosed with IgG4-RD, after presenting with a pancreatic mass, who was subsequently diagnosed with sarcoidosis based on a biopsy of a mediastinal lymph node.
Case Presentation
A 57-year-old woman presented for an outpatient rheumatology consultation for a recurrent hive-like rash on her bilateral upper extremities. The rash had been present for two months. She also complained of arthralgias, with morning stiffness in her hands. She denied any associated pruritus, but stated the rash gave her a burning sensation. She experienced moderate relief with naproxen and cortisone cream.
She had a similar rash on her arms three years prior. A diagnostic evaluation at that time discovered a pancreatic mass concerning for pancreatic adenocarcinoma. Histopathologic examination of the mass following a partial pancreatectomy revealed a focal lymphoplasmacytic infiltrate and dense fibrosis with a focal storiform pattern (see Figure 1, above). Focal phlebitis was present without obliteration of the lumens. Paired with a marked increase of IgG4-positive plasma cells on immunostaining, a diagnosis of IgG4-RD was felt to be most likely. The patient was not referred to a rheumatologist at that time, and no additional treatment was pursued.
With the current presentation, a comprehensive review of systems did not uncover evidence of fever, chills, sweats and weight loss. Her family history was negative for psoriasis, inflammatory bowel disease and inflammatory arthritis. She denied any smoking history, but admitted to social alcohol use.
On physical exam, she was in no distress and had normal vital signs. Her salivary glands were enlarged, but not tender. Multiple non-blanching urticarial lesions were seen over both arms, without involvement of her legs. The musculoskeletal exam was normal, with no evidence of synovitis. A lung exam was clear throughout, and a cardiovascular exam revealed a regular heart rate and rhythm without murmurs, and normal pulses.
The initial laboratory evaluation revealed thrombocytosis with platelets of 517,000/uL (reference range [RR]: 140,000–400,000/uL), a white blood cell count of 6,000/uL (RR: 3,800–10,800/uL), hemoglobin of 14 g/dL (RR: 11.7–15.5 g/dL) and hematocrit of 42% (RR: 35.0–45.0%). She had an elevated total cholesterol level of 266 mg/dL (normal <200 mg/dL) and increased fasting glucose of 162 mg/dL (RR: 65–99 mg/dL). The C-reactive protein (CRP) was elevated at 14.3 mg/L, but the erythrocyte sedimentation rate (ESR) was normal at 8 mm/hr (normal: <30 mm/hr). The complete metabolic profile, including chemistries and liver function, was within normal ranges. Amylase, lipase, calcium and vitamin D metabolites were within normal ranges.