RB underwent an open left nasosinus biopsy using a canthal approach. During the procedure, a large amount of necrotic material was encountered that extended into the bone with destruction of the left lamina papyracea. His sinus cultures grew moderate coagulase-negative staphylococcus and rare Clostridium birefrementas, which were felt to be colonizers. Sinus biopsies demonstrated chronic inflammation and several giant cells without granulomas or vasculitis.
Subsequently, RB underwent cystoscopy, which demonstrated a necrotic urethra with the process affecting the bladder base. Biopsies of the urethra and bladder revealed acute and chronic inflammation with necrosis without evidence of malignancy or infection.
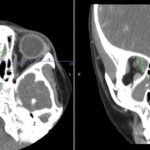
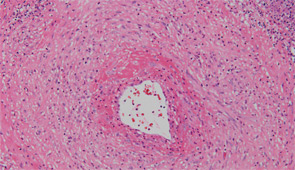
After sputum samples were negative for acid-fast bacilli on three consecutive days he underwent video-assisted thoracoscopic lung biopsy of the area encompassing the cavitary lung lesion. During the procedure the lesion was found to contain pus. Cultures of the abscess were negative. Microscopic examination of the lung specimen demonstrated granulomatous vasculitis without acid-fast bacilli or fungal elements consistent with granulomatosis with polyangiitis (GPA) (Wegener’s) (see Figure 4). Repeat head imaging demonstrated air-fluid collections underlying the left frontal sinus and in the middle cranial fossa inferior to the foramen rotundum measuring 1.3 cm by 0.5 cm. The infectious disease consultants felt that these were likely postoperative changes; however, broad spectrum antibiotics were recommended for two weeks.
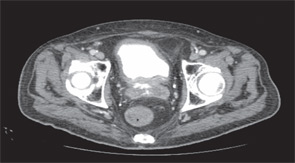
The patient was started on a two-day course of intravenous glucocorticoids followed by prednisone 60 mg daily and received two infusions of rituximab 1,000 mg given two weeks apart. His headaches and fatigue improved and his weight loss stabilized. Three weeks after hospital discharge he was hospitalized because of an episode of Clostridium difficile colitis that resolved with metronidazole treatment. He improved slowly but continued to have drainage from the canthal incision. He was followed by the ear, nose, and throat service, who felt there was no clear evidence of infection. Three months after hospital discharge, he underwent routine follow-up head imaging that revealed a markedly enlarged intracranial-fluid collection. He was taken emergently to surgery where a 3 cm by 3 cm brain abscess was evacuated. Cultures grew Aspergillus fumigatus. Despite treatment with liposomal amphotericin, voriconazole, and multiple debridements, his condition continued to deteriorate and, after a four-week hospital course, his family opted for comfort measures only.
Discussion
This case illustrates several important points regarding the diagnosis and treatment of GPA. For RB, the diagnosis of GPA was delayed by several months because of repeated negative ANCA testing and having several superimposed infections, which can mimic some of the upper airway disease that can be seen in patients with GPA.