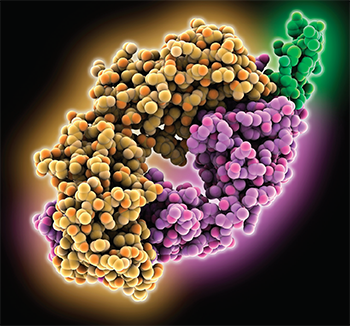
Computer model showing the
structure of the rituximab fab light chain (yellow) and heavy chain (purple) complexed with the B-lymphocyte antigen CD20 (green).
LAGUNA DESIGN / Science Source
Researchers sought to identify predictors of patients with anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV) who took rituximab for maintenance had a better sustained remission rate through 60 months than those taking azathioprine, according to the latest results from the maintenance of remission using rituximab in systemic ANCA-associated vasculitis (MAINRITSAN) trial, a prospective, randomized trial by the French Vasculitis Study Group.1
Rituximab proved superior to azathioprine for remission maintenance through 28 weeks, according to earlier findings from the trial, and rituximab’s relapse rate remained better through week 60.
“Rituximab had a superior post-treatment efficacy than azathioprine at maintaining remissions of ANCA-associated vasculitides over 60 months,” says Benjamin Terrier, MD, PhD, the lead author and consultant of internal medicine at Paris Descartes University, Paris, France. “Rituximab had superior benefit and no safety differences with azathioprine.”
Anisha Dua, MD, MPH, director of the Vasculitis Center at the University of Chicago, did not participate in the study, but she says the results affirm rituximab should play a significant role in maintenance.
“These findings support the efficacy of rituximab 500 mg infusions every six months as superior to azathioprine at 60-month follow-up in new and relapsing patients with GPA and MPA,” she says, referring to granulomatosis with polyangiitis and microscopic polyangiitis, respectively. “The side effect profile was comparable, but the rate of relapse was lower in the rituximab treated group. In practice, the implications are that we should really consider using rituximab therapy for maintenance in our patients with GPA and MPA.”
The experts note that an increased number of patients taking rituximab suffered major relapses after the 28-week mark—more than in the azathioprine group—which they say underscores the need to fine-tune maintenance strategies for the disease, including trying to identify patients for whom longer treatment durations may prove beneficial.
Nearly the same number of patients suffered severe infections in each group.
The Study Details
In the trial, researchers enrolled 115 patients with newly diagnosed or relapsed granulomatosis with polyangiitis, microscopic polyangiitis or renal-limited ANCA-associated vasculitis. They were all in complete remission after being treated with glucocorticoids and cyclophosphamide.

Dr. Dua
Patients were randomized to either receive rituximab, with two early doses of 500 mg and then doses at Months 6, 12 and 18, or azathioprine, with 2 mg/kg per day for 12 months, then 1.5 mg/kg per day for six months, then 1 mg/kg per day for four months. Decisions on prednisone dose tapering and stopping prednisone after 18 months were left to the investigators at each center. Prophylaxis with co-trimoxazole was recommended for patients with fewer than 250 CD4-positive T cells per mm3.
Investigators reported earlier that at 28 months, 17 patients in the azathioprine group suffered a major relapse; that is, a reappearance or worsening of the disease with one major organ involved or some life-threatening manifestation. That compared to just three major relapses in the rituximab group. Nine patients in the azathioprine group suffered a minor relapse.
Between months 28 and 60, 11 patients suffered a major relapse in the azathioprine group among those who’d been major relapse free, while 13 in the rituximab group suffered a major relapse. Three and seven patients suffered minor relapses, respectively.
At 60 months, the major relapse-free survival rate was 49.4% in the azathioprine group and 71.9% in the rituximab group (P=0.003). The completely relapse-free rate was 37.2% and 57.9% (P=0.012), respectively.
Nearly the same number of patients suffered severe infections in each group—16 for azathioprine and 15 for rituximab—but there were more instances of severe infection in the rituximab group (31) compared with the azathioprine group (20). Most of the infections were respiratory, and those were also more frequently seen in the rituximab group, including 10 cases of bronchitis compared to just one in the azathioprine group.
Three patients developed Pneumocystis jiroveci pneumonias, with none of the patients on prophylaxis at the time of infection—one because it had been discontinued, one due to allergy and poor compliance with a substitute, and another due to allergy. Experts say this highlights the need for clinicians to emphasize prophylaxis to their patients.
An analysis showed those on rituximab went 12.6 more months without a relapse or toxicity than those taking azathioprine (P<0.001).
Dr. Terrier says that despite rituximab’s superiority over five years, the increased number of relapses in the group shows the need to continue to improve maintenance treatment.
“Rituximab could delay rather than abrogate relapses,” he says.