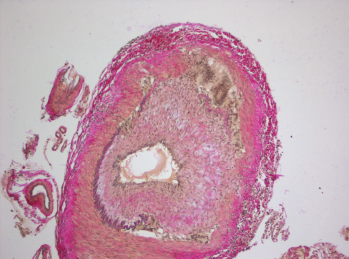
Histopathology of giant cell arteritis in a temporal artery.
wikimedia.org
A recent study, conducted by the Vasculitis Clinical Research Consortium and funded by the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS), examined whether the addition of abatacept, a drug that affects T cell activation, to standard prednisone treatment could reduce the risk of relapse in patients with giant cell arteritis (GCA).1 Although abatacept has been approved by the FDA to treat rheumatoid and juvenile idiopathic arthritis, there had been no prior experience with its use as a treatment option for GCA.
Carol Langford, MD, MHS, of the Center for Vasculitis Care and Research at Cleveland Clinic, and the study’s lead investigator, discussed the reasons why the study of abatacept was pursued in GCA: “Abatacept inhibits T cell activation, which is thought to play a critical role in the pathogenesis of GCA,” Dr. Langford says. “Because of this mechanism, its favorable safety profile in rheumatoid arthritis and the unmet need for additional treatment options in GCA, abatacept was an interesting drug to investigate.”
Nature & Treatment of GCA
According to Dr. Langford, GCA is an inflammatory disease typically seen in older adults that affects the large blood vessels, leading to a narrowing or blocking of the vessels, which interrupts blood flow. When this affects branches of the internal or external carotid artery, this can manifest with headaches, jaw or tongue claudication, scalp tenderness or cranial ischemic complications, such as vision loss, scalp infarction or strokes.
GCA can also be associated with thoracic aortic aneurysms, according to Dr. Langford, which can occur primarily or as a late manifestation of disease. The condition is commonly associated with polymyalgia rheumatica (PMR), an inflammatory disorder that causes aching and stiffness along the shoulder and hip girdle. PMR can occur as an isolated entity or as part of the clinical spectrum of GCA.
Although no uniformly applied treatment protocols exist for GCA, Dr. Langford says an initial dose of prednisone equivalent to 40–60 mg/day is commonly used, with higher doses being considered for cranial ischemic complications.
Glucocorticoids relieve symptoms and, importantly, can prevent blindness, but Dr. Langford says relapses are common in GCA patients, which lead to prolonged glucocorticoid exposure.
“Relapses in GCA are a concern not only because of the potential for disease-related organ damage, but also due to the need for prolonged glucocorticoid treatment,” Dr. Langford says, adding that side effects of glucocorticoids can include infection; osteoporosis; diabetes; cataracts; glaucoma; fluid retention, causing swelling in the lower legs; high blood pressure; problems with mood, memory, behavior and other psychological effects; and weight gain, with fat deposits in the abdomen, the face and the back of the neck.

