SNOWMASS VILLAGE, COLO.—The study of anti-neutrophil cytoplasmic antibody (ANCA) associated vasculitis (AAV) is ongoing, and research results should help improve treatment for this patient population. Key trials and therapeutic options were discussed at the 2020 ACR Winter Symposium during the session, Update on the Treatment of ANCA-Associated Vasculitis, by Peter A. Merkel, MD, MPH, chief of the Division of Rheumatology, director of the Penn Vasculitis Center, and professor of medicine and epidemiology at the University of Pennsylvania.
“This past year has seen the release of the results of several major trials that will change the standard of care for patients with [AAV],” Dr. Merkel said. “These new data will be of great interest and relevance to practicing rheumatologists.”
Standard of Care
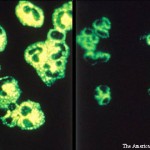
AAV is a group of diseases characterized by the destruction and inflammation of small- and medium-caliber vessels and includes microscopic polyangiitis (MPA), granulomatosis with polyangiitis (GPA) and eosinophilic granulomatosis with polyangiitis.
Although treatment for AAV has advanced substantially in the past few decades, there are still many unmet needs. In particular, less toxic regimens, more rapid induction of remission and prevention of relapse remain important research goals.
Current therapy for non-severe disease includes combining glucocorticoids with methotrexate or rituximab. For more severe disease, therapy options include:
- Combining glucocorticoids with rituximab or cyclophosphamide, followed by maintenance of remission with any of several agents, including rituximab, azathioprine or methotrexate;
- Plasma exchange, which has been highly controversial; and
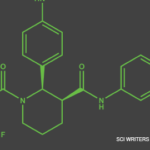
- Novel agents, especially inhibitors of C5a, trials of which have been highly encouraging.
Key Multi-Center Trials
The 2014 MAINRITSAN study was an open-label, randomized, controlled trial that included 115 patients with AAV who attained remission after treatment with cyclophosphamide and glucocorticoids.1 Patients were randomized to receive rituximab (500 mg intravenously) or azathioprine (which was tapered at one year). Results showed more patients had sustained remission at 28 months with rituximab than azathioprine.
After this study, several questions remained to be investigated, Dr. Merkel said. Key among them: What about patients who didn’t receive cyclophosphamide for induction? Will lower-dose glucocorticoids work as well? What predicts relapse or sustained remission?
After MAINRITSAN, studies have looked into some of these and other questions to help elucidate the therapeutic potential of existing and emerging treatments.
RITAZAREM was an open-label, randomized, controlled trial that compared rituximab with azathioprine as a maintenance therapy in relapsing AAV for 190 patients with GPA/MPA who were enrolled during a relapse of their vasculitis and treated with rituximab.2 At four months, 170 patients attained remission and then were randomized to different treatment groups: 85 patients received maintenance treatment with 1,000 mg of rituximab every four months, and 85 received azathioprine 2 mg/kg/day. In addition, patients’ glucocorticoid doses were tapered. Treatment ended at month 24 with follow-up out to 36–48 months.
Initial results of RITAZAREM, presented at a plenary session at the 2019 ACR/ARP Annual Meeting, showed that rituximab was superior to azathioprine for preventing disease relapse in AAV patients with a prior history of relapse.3 The study didn’t uncover any new major safety signals for use of these medications in this population either, said Dr. Merkel, one of the two principal investigators of the international trial.
“The results of the MAINRITSAN and RITAZAREM [trials] firmly establish the role of rituximab in maintenance of remission in AAV,” Dr. Merkel said.