Subgroup 3
The group evaluated the possibility of using results of aPL antibody tests to calculate “risk factors” for APS-related clinical manifestations. Otomo and colleagues have described an antiphospholipid score (aPL-S), a weighted summation of results from LAC, aCL, anti-β2GPI, and anti–phosphatidylserine/prothrombin (anti–PS/PT) assays based on odds ratios. A higher prevalence of APS clinical manifestations was observed in patients with higher aPL-S, suggesting the use of a cluster analysis in the future to predict an APS risk factor. Also, when considering groups of tests, the risk of APS was found to be calculated as higher if the data were analyzed by cluster analysis or by combining the results of more than one test (aCL, anti-β2GPI, LAC).
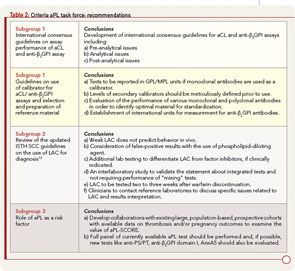
Based on the limited data available to establish the use of aPL antibody tests as risk factors, the task force supported the idea of deriving a risk factor score but recommended expanding or confirming these preliminary observations by identifying and developing collaborations and by conducting studies with existing large, population-based, prospective cohorts with available data on thrombosis and/or pregnancy outcomes. In addition, the task force recommended that a full panel of current aPL antibody tests be included in any one of those studies (i.e., aCL and anti-β2GPI immunoassays and LAC assays). Furthermore, new tests such as antiprothrombin, anti–PS/PT, anti-β2GPI domain I, and annexin A5 (AnxA5) resistance (discussed below) should be studied as well.9
Noncriteria APL Tests: Hope for a Better Future on APL Testing?
As indicated above, the revised classification criteria for the diagnosis of APS includes positivity of at least one of the three criteria aPL antibody tests.7 However, the use of these tests may not guarantee full sensitivity and specificity to confirm an APS diagnosis. In clinical practice, there are indeed many “false positives” with aPL antibody tests, especially with the aCL ELISA, which can give positive results in clinical conditions aside from APS; these conditions include infectious diseases (e.g., syphilis), malignancies, and other autoimmune diseases. However, there are patients with clinical patterns strongly suggestive of APS but who are persistently negative for criteria tests. Additionally, the criteria aPL antibody tests may not identify “pathogenic” subpopulations of aPL antibodies.
Several autoantibodies have been demonstrated to bind directly to negatively charged phospholipids other than cardiolipin (individually or as a phospholipid mixture) or to other proteins in the coagulation cascade (i.e., prothrombin and/or phosphatidylserine-prothrombin complexes); antibodies can also interfere with anticoagulant activity of the AnxA5. However, the clinical and diagnostic utility of these newly developed assays as well as their standardization requires much further study. In some cases, these new assays lack standardization, and there are not international units of measurements.