Angiography-negative primary central nervous system vasculitis in children: A newly recognized inflammatory central nervous system disease. (Arthritis Rheum. 2005;52:2159-2167.)
Abstract
Inflammatory central nervous system (CNS) diseases in childhood comprise a wide spectrum of heterogeneous conditions. We studied four children with primary CNS vasculitis in whom results of magnetic resonance imaging studies were abnormal but results of conventional angiography were normal. We determined that angiography-negative, biopsy-confirmed primary small-vessel CNS vasculitis is a previously unrecognized distinct disease entity in children. The diagnosis must be considered in a child with a progressive, acquired diffuse or focal neurologic deficit, even if the results of conventional angiography are normal. A lesional brain biopsy is required to confirm the diagnosis. Use of immunosuppressive therapy plus aspirin leads to an excellent neurologic outcome.
Primary central nervous system vasculitis presenting with intracranial hemorrhage. [abstract]. (Arthritis Rheum. 2010;62(Suppl 10):2037.)
Objective: Primary central nervous system vasculitis (PCNSV) is an uncommon and heterogeneous condition that affects the brain and spinal cord. This study was undertaken to evaluate the clinical features and outcomes of patients who presented with intracranial hemorrhage (IH) in the context of the largest cohort of consecutive patients with PCNSV studied to date.
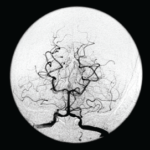
Methods: We identified 131 consecutive patients with PCNSV seen over the 25-year period of 1983 to 2007. PCNSV diagnoses were based on findings from a central nervous system (CNS) biopsy or conventional angiography (or both). We compared patients presenting with IH (within three months of the date of PCNSV diagnosis) to those without. We evaluated data on demographics, clinical findings, laboratory studies, imaging, biopsy of brain or spinal cord (or both), treatment and neurologic outcome.
Results:Sixteen (12.2%) cases had IH at presentation. Twelve patients had intracerebral hemorrhage (ICH), and four subarachnoid hemorrhage. Cerebral angiography was performed in 13 patients and showed multiple-vessel vasculitic changes in all. CNS biopsy findings were positive in four patients. Three patients had an acute necrotizing pattern, one had a granulomatous inflammatory pattern. Amyloid angiopathy was observed in 2 biopsy-positive specimens.
Compared with the 115 patients without, the 16 patients presenting with IH were more frequently females (100% versus 50.4%, p<0.001), persistent neurological deficit or stroke (12.5% versus 42.6%, p=0.027) and altered cognition (25% versus 56.5%, p=0.030) occurred less frequently, and the frequency of patients who had discontinued therapy by the last follow-up visit was higher (37.5% versus 14.2%, p=0.031). MRI and angiographic findings (excepted the presence of ICH), type of therapy (corticosteroids only or associated to immunosuppressive agents), therapy duration, frequencies of relapses, cerebrospinal fluid abnormalities, and Rankin disability score at last follow-up were similar. The survival curves of patients with and without IH were not different.