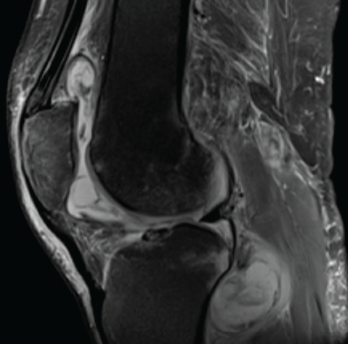
Figure 1. Magnetic resonance imaging of the patient’s left knee shows joint effusion, synovial thickening, and periarticular muscle and soft tissue edema.
Tumor necrosis factor-α inhibitors (TNFi’s) have emerged as an integral part of therapeutic strategies for several rheumatic diseases. TNF-α is a pro-inflammatory cytokine implicated in the pathogenesis of rheumatoid arthritis (RA), seronegative spondyloarthropathies and inflammatory bowel disease (IBD). It also plays a central role in the immune response to mycobacterial infection.
Many biologic agents, particularly TNFi’s, are associated with an increased risk of tuberculosis; however, the risk of non-tuberculous mycobacterial infections among patients treated with a TNFi has not been studied extensively.
We present this report on a patient with sarcoidosis receiving TNFi therapy who developed a disseminated non-tuberculous mycobacterial infection.
Case History
A 69-year-old man presented to the clinic with symptoms of progressively worsening left knee pain, stiffness and swelling over six months. He was unable to bear weight on the affected leg and was wheelchair bound. He had previously been diagnosed with both neurosarcoidosis and osteoarthritis. He had initially been treated with glucocorticoid monotherapy. Because he deteriorated clinically, 400 mg of intravenous (IV) infliximab every six weeks and 500 mg of mycophenolate mofetil twice a day orally were added to his medical regimen.
His knee had initially been evaluated by his primary care provider; plain radiographs of the knees demonstrated osteoarthritis. Subsequently, he was referred to a sports medicine specialist and an orthopedic surgeon for further evaluation. Oral analgesics, intra-articular steroid injection and physical therapy provided him with no relief, and he was referred to our division for further evaluation.
In our clinic, he was afebrile; his blood pressure was 152/82 mmHg, and his heart rate was 66 bpm. His left knee was swollen, and both passive and active movements were limited by pain.
Laboratory tests on his initial presentation demonstrated leukocytosis; his white blood cell count was 13,200/uL with 86% neutrophils. His complete metabolic panel and urinalysis were unremarkable. Rheumatoid factor, anti-cyclic citrullinated protein antibodies and anti-double stranded DNA antibodies were not detected on immunological studies. Tests for Borrelia and Coccidioides IgG and IgM antibodies were negative.
Magnetic resonance imaging (MRI) of the left knee joint revealed a moderate joint effusion with diffuse synovial thickening, and periarticular muscle and soft tissue edema (see Figure 1, above).
Synovial fluid aspirate demonstrated 8,935 nucleated cells (70% mononuclear) with Mycobacterium avium-intracellulare growth in modified Middlebrook 7H9 broth, a liquid growth medium used to culture Mycobacterium.
Infliximab was stopped, and the patient was treated with ethambutol and azithromycin.
Over the next month, the patient noticed low-grade fever, malaise, night sweats and unintentional weight loss of 10 lbs. He underwent open synovectomy of the left knee. The synovial tissue demonstrated an active granulomatous synovitis (see Figure 2, and synovial cultures grew Mycobacterium avium complex (MAC).