The following report outlines a case of newly diagnosed adult-onset Still’s disease (AOSD) complicated by macrophage activation syndrome (MAS) in a previously healthy and active 32-year-old man who had emigrated from Africa to the U.S.
The following report outlines a case of newly diagnosed adult-onset Still’s disease (AOSD) complicated by macrophage activation syndrome (MAS) in a previously healthy and active 32-year-old man who had emigrated from Africa to the U.S.
Case
A man with no prior medical history presented with acute-onset polyarthritis, fevers and fatigue that began one month previously. He had been seen in the emergency department several times and had multiple visits to his primary care doctor, who also noted elevated inflammatory markers.
In addition to the arthritis, he had developed a transient, diffuse rash and gross hematuria one week earlier. A review of systems also revealed sore throat, cough, pleuritic chest pain, muscle weakness, and an inability to walk. His symptoms were not relieved by ibuprofen.
On physical exam, the patient appeared ill, in mild distress and was sitting in a wheelchair. The patient had active synovitis, with notable red, hot, swollen joints in his fingers, knees, ankles and wrists. He had difficulty making a fist with both hands. The patient was prescribed 60 mg of prednisone daily and instructed to follow up in one week to review the results of his laboratory tests.
Laboratory results: elevated AST 170 U/L (normal range: 17–59 U/L), ALT 135 U/L (normal range: 0–57 U/L), albumin 3.2 g/dL (normal range: 3.5–5.0 g/dL) white blood cell count 23.2K/mcL (normal range: 4.5–11K/mcL) with 96% polymorphonuclear neutrophils (PMN), erythrocyte sedimentation rate (ESR) 37 mm/hr (normal range: 0–15 mm/hr), C-reactive protein (CRP) 328.2 mg/L (normal range <10 mg/L). Most notably, ferritin was significantly elevated at 20,853.3 ng/mL (normal range: 3.8–10.6 ng/mL).
Due to these markedly abnormal lab results and lack of improvement with high-dose glucocorticoids, the patient was directly admitted to the hospital for further evaluation. Specialists in infectious disease, rheumatology, oncology and orthopedic surgery followed this patient during his hospitalization.
Extensive infectious disease testing was performed, ruling out SARS-CoV-2, hepatitis B, hepatitis C, HIV, cytomegalovirus, Epstein-Barr virus, parvovirus B-19, influenza, malaria, histoplasmosis and tuberculosis. Blood and urine cultures were negative. Uric acid levels, rheumatoid factor and antistreptolysin O antibodies were within normal limits. Chest X-ray, computed tomography (CT) of the chest, abdomen and pelvis, and magnetic resonance imaging (MRI) of the cervical, thoracic and lumbar spine revealed no acute pathology, signs of infection or masses. Transthoracic echocardiogram was negative for valvular vegetation.
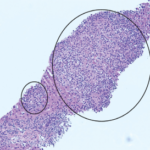
On hospital day 3, synovial fluid analysis of the left knee revealed some calcium pyrophosphate crystals.