A 44-year-old woman presented to the emergency department with bifrontal headaches that had started approximately one month earlier. She was diagnosed with migraines and discharged home. Three days later, the patient returned to the emergency department upon recurrence of her headaches, and this time she also reported abnormal leg movements. A computerized tomography (CT) scan and magnetic resonance imaging (MRI) of the head were unrevealing.
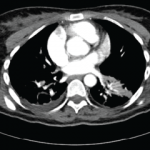
The patient’s symptoms appeared to be due to a transient ischemic attack, and she was treated with warfarin with instructions to follow up with a neurologist. On follow-up, the neurologist ordered a repeat MRI of the brain. While at the MRI facility a few days later, the patient began to have severe headaches again and was sent back to the emergency department. The MRI showed nonspecific white matter changes from the midbrain to the thalamus. She was started on 1 g of intravenous (IV) methylprednisolone and admitted to the hospital.
On further investigation, the patient reported that she had recurrent oral ulcers once per month. The lesions were singular in nature and had never appeared in clusters. A rheumatologist was consulted to evaluate for Behçet’s disease, but the evidence was felt to be insufficient; she did not report any changes in vision, genital ulcers, joint pain or morning stiffness. She had no evidence of uveitis, oral ulcers, genital lesions, rashes or pathergy on exam.
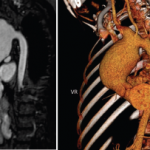
A positron emission tomography scan revealed a calcified granuloma in the left lower lobe of the lung. This finding prompted the neurologist to consider neurosarcoidosis. The patient was discharged on 60 mg of prednisone daily with plans for steroid taper managed by the neurologist.
On follow-up with the neurologist three months later, the patient was on 26 mg of prednisone daily and was doing well.
Two months after that visit, she presented to the emergency department again, this time reporting two weeks of difficulty speaking and an unsteady gait. She reported new skin lesions over her chest and both arms, which had developed within the prior month, and an increased frequency of oral ulcers. She also complained of confusion and an inability to focus at work. She denied arthritic symptoms at the time of presentation but did report right ankle pain and swelling approximately two to three weeks prior. By this time, she was on 6 mg of prednisone daily.
Her physical exam was significant for oral aphthous lesions, painful erythematous nodules over the left upper lateral and medial shin, and reddish-brown raised plaques on her anterior chest and both upper extremities (see Figures 1–3). She had swelling and tenderness over her proximal interphalangeal joints and metacarpophalangeal joints of both hands, as well as synovitis in both ankles. She was speaking with a lisp, had an unsteady gait and spastic choreiform-like movements of both legs. No sensory deficits were experienced, and her strength remained intact throughout the exam.