Diagnosis
Crusted scabies, formerly known as Norwegian scabies, is an uncommon parasitic infection caused by infestation of the superficial layers of the skin with the mite, Sarcoptes scabiei var hominis.1 The name Norwegian scabies originates from its first description in 1848 of a group of Norwegian leprosy patients who developed the crusted scabies variant.2
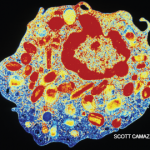
Unlike typical scabies, crusted scabies requires an inadequate host response to the arthropod mite, leading to a hyperinfestation state, with up to 2 million mites per person.3,4 This presentation usually occurs in patients with compromised immune systems, such as those on immunosuppressive therapy, infections with HIV or HTLV-1, or those with severe debilitation or cognitive dysfunction.1,5 Pruritis, caused by an allergic response to the mites within the skin, is a common manifestation of infection, which can lead to the diagnosis. However, in the immunocompromised patient, this urge to itch may be absent due to an altered immune response, which allows for heavy infestation.3,4
Crusted scabies is highly contagious and can be spread by minimal contact or indirect transmission through clothing or bedding. Classic scabies usually requires prolonged person-to-person contact and is rarely spread without direct contact.1 A classic infection of scabies has a mite load of about 10–15 mites per person; however, in crusted scabies, there are millions of mites underneath the skin, causing a crusted, scaly or even warty hyperkeratotic appearance of the skin.1,3
The presentation of crusted scabies is commonly limited to an isolated region of the body, such as the palms and soles, but infrequently involves the scalp. This atypical presentation can mimic many other conditions (e.g., dermatomyositis, psoriasis, discoid lupus) resulting in a delay in diagnosis.5 Prompt recognition of the condition is necessary because an outbreak can spread to those working close to the infected individual or even progress to an institution-wide infestation, as reported in our case.3 There is also heightened risk for secondary infections that could potentially lead to a life-threatening sepsis.2
The diagnosis of crusted scabies requires direct visualization of the mite with a light microscope under low power; however, false negatives can occur.
The diagnosis of crusted scabies requires direct visualization of the mite with a light microscope under low power; however, false negatives can occur. A mite may be visualized on a skin biopsy as well.1 Treatment for crusted scabies includes topical keratolytic therapy, topical scabicides and a multidose regimen of ivermectin depending on the severity of the condition.3,6