The patient was referred to a pulmonary specialist, who performed diaphragmatic ultrasound. The ultrasound revealed both reduction in diaphragm dome excursion and in diaphragm thickening fraction, consistent with bilateral diaphragm dysfunction, confirming diaphragmatic dysfunction and a diagnosis of shrinking lung syndrome (see Figure 1). Follow-up high-resolution CT showed no evidence of interstitial lung disease. Mycophenolate mofetil was initiated, in addition to prednisone.
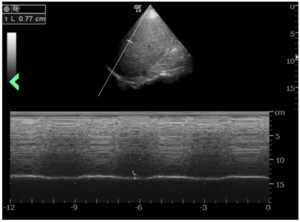
Figure 1: The ultrasound revealed a reduction in diaphragm dome excursion of 0.77 cm (normal value for deep inspiration: 4.8 cm) and in diaphragm thickening fraction, consistent with bilateral diaphragm dysfunction. (Click to enlarge.)
Repeat PFTs three months later demonstrated improvement, with FVC post 39%, FEV1 post 37%, FEV1/FVC post 92% predicted, TLC 50%, DLCO 38%, reduction in mean inspiratory pressure and decline of vital capacity from a seated to supine position.
Discussion
Diagnosis of shrinking lung syndrome usually follows the diagnosis of SLE, with a mean interval of 66.7 months.2 This case is atypical because shrinking lung syndrome was part of the initial presentation of systemic lupus erythematosus. This added to diagnostic uncertainty in this case.
It is important to highlight the role of ultrasonography of the diaphragm in our case, which confirmed diaphragm involvement and assisted us in making the diagnosis of shrinking lung syndrome. Upon our patient’s initial presentation to the hospital, there was concern for a possible overlying acute process, such as neumonia. Although additional CT scans showed resolution of parenchymal lung abnormalities, the patient continued to have severe dyspnea. Subsequent PFTs showed restrictive lung defect and resulted in an unclear clinical picture.
Fortunately, ultrasonography is a noninvasive and rapid bedside test that can provide real-time data on diaphragmatic function without subjecting patients to radiation. It has a sensitivity and specificity of more than 90% for diagnosis of diaphragmatic dysfunction.3-5 Real-time ultrasound in this case confirmed diaphragmatic dysfunction and enabled immediate initiation of immunosuppressive therapy, rather than waiting for repeat chest imaging.
Although the exact pathogenesis of shrinking lung syndrome is unclear, several hypotheses have been proposed, including that it may result from surfactant deficiency, isolated diaphragmatic myopathy, phrenic neuropathy, chest wall dysfunction or pleural adhesions.6
Recent data suggest that shrinking lung syndrome may be a complication of pleural inflammation. Inflammation, particularly around the regions of the diaphragmatic pleura or a pleural region near the diaphragm, could lead to chronic lung hypoinflation and loss of compliance due to activation of local neuroreflexes, which inhibit diaphragm function and eventually cause diaphragmatic remodeling.7



