Dr. Joste
A follow-up positron emission tomography (PET) scan demonstrated persistence of the left neck mass and an unexpected retroperitoneal area of involvement. A bone marrow biopsy revealed normal cellular trilineage hematopoiesis, and flow cytometry showed a lambda-restricted plasma cell population by CD138 immunostain estimated to be 5–9% plasma cells consistent with AL-type amyloid, although no overt evidence of amyloid was observed in the bone marrow.
Our patient was diagnosed with an unusual nodular AL amyloid with two areas of involvement (including his left neck and a retroperitoneal area) without a predisposing systemic autoimmune or rheumatologic condition.
Following the amyloidosis diagnosis, the patient was evaluated by a hematologist and an oncologist, who devised a treatment plan consisting of the administration of subcutaneous bortezomib along with dexamethasone on a weekly basis three of four weeks each month.
A transthoracic echocardiogram performed to assess possible cardiac involvement revealed a mild reduction of left ventricular systolic function with a calculated ejection fraction of 49%, as well as a transmitral spectral Doppler flow pattern suggestive of mild diastolic dysfunction, with normal left ventricular end diastolic pressure and mild global hypokinesis of the left ventricle. At press time, the patient had yet to obtain further cardiac evaluation regarding these findings.
Given the paucity of data regarding management of such an uncommon presentation of amyloidosis, expertise from specialists at the Mayo Clinic, Scottsdale, Ariz., was sought. The hematologist and oncologist believed the patient may be a candidate for an autologous stem cell transplant in the future.
The patient’s right hip osteoarthritis, with prior hip replacement with revision surgery, was most likely mechanical in origin, stemming from prior physical activity rather than an underlying systemic disease. For this, we recommended he continue conservative management using non-steroidal anti-inflammatory drugs and pursue activity only as tolerated.
Finally, the thyroid nodule initially noted on the CT scan and subsequently determined on fine needle aspiration to be consistent with Hashimoto’s thyroiditis was determined to be best monitored by the endocrinology service.
Discussion
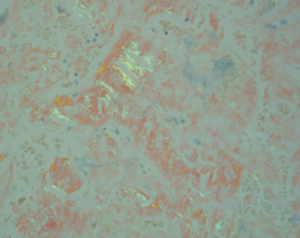
Figure 2. This image shows fibrous tissue with apple-green birefringent material consistent with the presence of amyloid (H&E, 400x).
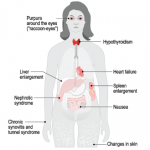
Amyloidosis is a condition consisting of several distinct clinical entities sharing the common pathological feature of protein misfolding, resulting in fibrils consisting of a highly structured, stable, beta-sheet confirmation prone to binding with other like molecules. Upon visualization of amyloid tissue stained Congo red under polarized microscopy, one can appreciate a highly characteristic apple-green birefringence appearance.
Although the most common forms include AL (primary) and AA (secondary) amyloidosis, other forms include dialysis-associated, age-related, heritable forms and organ-specific amyloid with multiple deposits. The secondary AA form often appears with several rheumatologic conditions, including rheumatoid arthritis, chronic juvenile polyarthritis, ankylosing spondylitis, psoriatic arthritis, dermatomyositis, systemic lupus erythematosus, systemic sclerosis and Sjögren’s syndrome, in addition to a number of chronic inflammatory conditions, including inflammatory bowel disease, familial periodic fever syndromes, chronic infections and certain neoplasms.1
Although the systemic form is seen most often and localized presentations occur less frequently, organ-specific deposits may also be observed, such as Alzheimer’s disease deposition in the aging brain or type 2 diabetes deposits in the islets of Langerhans.2 Somewhat less commonly encountered organ-specific deposits include isolated bladder amyloidosis, in addition to localized hepatic forms.
In contrast, localized AL amyloid appears much less frequently and may present as a localized tumor-like nodule or a collection of several nodules. Symptoms vary due to the location of presentation or the structures affected. With such localized presentations, the specter of malignancy is often lurking, particularly when the breast, lung and urinary tract are involved. The most frequently encountered sites of localized AL amyloid deposition include the eyelids, skin, bronchi, larynx and urinary tract.2
In our case, the presentation of localized AL amyloid in the neck was found to involve several structures, including blood vessels, a lymph node and subcutaneous tissue. Additionally, the calcifications visualized on CT imaging were highly suspicious for cancer, particularly given the context of a noted hyper-functioning thyroid nodule; metastatic lymphadenopathy from a primary thyroid malignancy was of legitimate concern. Calcifications commonly appear in nodular presentations of AL amyloid, and microcalcifications are often identified when breast tissue is involved. When such microcalcifications appear on mammography, concern for cancer is heightened.2