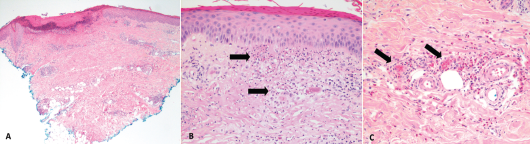
Figure 2. These hematoxylin and eosin stain images show the patient’s histology of RCEV demonstrating vasculitis, including image A, a biopsy from her right leg showing ulceration and superficial and deep perivascular inflammation with vascular damage (magnification 40X); B, a biopsy from her left leg showing cutaneous small vessel vasculitis (the arrows indicate examples of damaged blood vessels) with fibrinoid necrosis of vessel walls and surrounding nuclear debris/leukocytoclasis (magnification 200X); and C, a biopsy from her right leg showing small vessel vasculitis (arrows), uninvolved adjacent small arterioles and abundant perivascular and interstitial eosinophils (magnification 200X).
Discussion
RCEV was initially described by Chen et al. in 1994 and is characterized clinically by its benign course and classically pruritic skin eruptions. Various skin morphologies have been noted with RCEV, including urticaria, papules, patches, nodules, angioedema and vesicles.1-9 Only one previous group has described RCEV with ulcerating lesions, as we saw in this case.8 The lack of peripheral eosinophilia noted in our case was also unique, and this feature was noted in only three of the 17 cases.4,6,9
Histology can reveal necrotizing vasculitis with predominant eosinophilic infiltration, and others have commented on the presence of neutrophils and lymphocytes.5,8,9 Granulomas and leukocytoclastic features are typically absent in RCEV, although our case did feature some evidence of leukocytoclasis on histology.1-9 A number of specific findings enabled us to rule out similar conditions, such as eosinophilic granulomatous polyangiitis (EGPA), urticarial vasculitis, Wells syndrome and hypereosinophilic syndrome (HES).
Classically, patients with EGPA have asthma, peripheral eosinophilia and leukocytoclastic vasculitis with granulomas on biopsy.10 Urticarial vasculitis typically presents with skin lesions that resolve with pronounced central clearing and hyperpigmentation, rather than vesicles and ulcers.11 Leukocytoclasia is also a key histological feature in urticarial vasculitis.11,12
Patients with Wells syndrome tend to have peripheral eosinophilia and granulomas with no features of vasculitis on biopsy.13 Finally, HES was unlikely in light of the normal bone marrow biopsy and absence of eosinophilia or visceral involvement.14
Despite some atypical features, our patient’s clinical and histological presentation were consistent with RCEV. Glucocorticoids effectively manage RCEV, but recurrence is common after tapering the dose.1-9,15 Some recommend initiation of oral prednisone at 0.5 mg/kg/day and tapering it at two weeks to reach the minimum necessary dose to maintain remission.16
However, only a few known cases of RCEV report successful withdrawal of systemic steroids.5-7 Sakuma-Oyama et al. described RCEV in a 27-year-old female maintained solely on 300 mg of suplatast tosilate daily, a medication also used in eczema and asthma management known to suppress immunoglobulin E, interleukin 4 and interleukin 5.5 Tanglertsampan et al. successfully treated RCEV with 150 mg of indomethacin daily.8 Another group used dapsone in conjunction with glucocorticoids to manage two patients with RCEV.15 Use of other immunosuppressive agents in the treatment of RCEV was described in only one case, in which 2 mg of oral tacrolimus daily allowed prednisone to be tapered.7
In our case, azathioprine actually provided some steroid-sparing benefit, and her prednisone dose was tapered to 5 mg daily. But unfortunately, gastrointestinal side effects (e.g., nausea and diarrhea) prohibited azathioprine’s use. Methotrexate and hydroxychloroquine proved ineffective. Tacrolimus in addition to methotrexate caused kidney injury. Further therapy escalation to stronger immunosuppression, such as mycophenolate or cyclophosphamide, has not been reported and was limited in this case due to recurrent urinary tract infections.