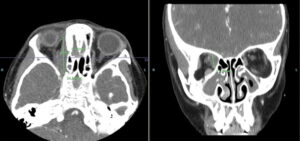
Sinus disease was also found within the right maxillary sinus, with complete obliteration and underlying periosteal thickening. Circumferential mucosal thickening, with aerated secretions within the left maxillary sinus extending into the left ethmoid infundibulum, was seen.
Due to these findings, the patient was admitted to the hospital for expedited evaluation by, and consultation with, both an otolaryngologist and an ophthalmologist.
Hospital Course
On admission—two months after her first emergency department visit—her physical examination showed proptosis of the right eye with slight edema, compared with the left eye. This was a new finding. Despite the proptosis and mild edema, extraocular movements were intact. She did have lymphadenopathy that was worse along the right side of her neck. Otherwise, the examination was unremarkable. During questioning, she said she began to have blurry vision while in the emergency department that day.
Magnetic resonance imaging (MRI) showed a right medial, orbital mass encasing the right trochlear and medial rectus muscles (see Figure 1). The mass was non-uniform, with variable signal intensity. Again, imaging favored a non-infectious inflammatory process over infection. Pansinusitis with osseous destruction of the medial maxillary sinus walls was visualized on the right. The laboratory testing was expanded to include IgG subclasses to evaluate for IgG4 disease; all IgG subclasses were elevated (see Table 1).
The patient underwent biopsies of both the sinuses and the orbit shortly after admission. The hematoxylin and eosin (H&E) stain from the sinus biopsy showed densely collagenous fibrotic background with focal chronic inflamAnmation including many plasma cells in three of five fragments. Small vessels, including arterioles, had concentric or periarterial fibrosis with edematous changes. Focal neutrophilic vasculitis was noted. Classic fibrinoid necrosis was not seen on the slides examined. No granulomas, fungi or viral inclusions were identified. No evidence of neoplasm or malignancy was seen.
The biopsy from the orbit showed dense fibrous and adipose tissue with focal, chronic inflammation. Findings were difficult to fully examine due to extensive crush artifact (i.e., damaged tissue caused by iatrogenic compression of the tissue during collection; it can often result from firm handling with forceps, fingers or other instruments). Despite this, the small vessels were revealed to have concentric or periarterial fibrosis with edematous change. No granulomas, fungi or viral inclusions were identified, and no evidence of neoplasm or malignancy was seen.
Both biopsies were reviewed with the pathologist, and the findings from both the sinus and ocular biopsies appeared to be part of the same underlying process and not two different etiologies. A diagnosis of IgG4-related disease was considered unlikely based on her immunohistochemistry and laboratory testing (see Table 1). Given the biopsy results, early ANCA-associated vasculitis was considered more likely. Based on her presentation, biopsies and laboratory values, the patient was subsequently diagnosed with GPA.