Alila Medical Media / shutterstock.com
Behçet’s disease is a chronic, relapsing and remitting vasculitis with multisystem involvement. Commonly referred to as the Silk Road disease due to its prevalence in the Asian and Mediterranean region of the traditional Silk Road, Behçet’s was first described by Hippocrates as a triad of symptoms—genital and oral ulcers with uveitis—and attributed to links with other illnesses. The Turkish physician Hulusi Behçet was the first to distinguish the freestanding symptoms as a disease manifestation of their own and came to describe Behçet’s disease. Behçet’s can affect arteries and veins of all sizes. When it involves the central nervous system and intestines, it results in a poorer prognosis. Current genetic and environmental links to the disease are being evaluated, including upregulation of HLA-B27 and heat shock protein 60 as well as association with herpes simplex virus and streptococcal virus.
The Case
A 34-year-old woman presented with a chief complaint of recurrent abdominal pain. She had a past medical history of Behçet’s disease with multiple abdominal symptoms and gastrointestinal involvement. Her past surgical history included an appendectomy and cholecystectomy. An abdominal X-ray was negative. Because of the patient’s history, she was admitted for abdominal pain control secondary to a Behçet’s flare.
She was started on a hydromorphone patient-controlled analgesia (PCA) along with continuing her home steroids and azathioprine. She was started on standard heparin subcutaneous injections for deep vein thrombosis prophylaxis while an inpatient. Three days into her hospital stay, the patient syncopized in the bathroom.
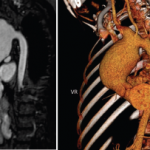
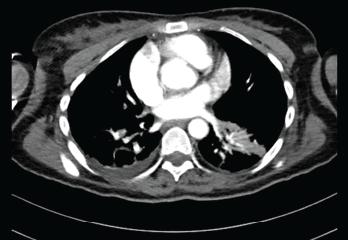
Vitals at the time showed a blood pressure of 70/40 with sinus rhythm. A computed tomography (CT) scan of the head was negative for an acute bleed. Her troponins continued to rise, peaking at 1.68. A transthoracic echocardiogram showed reduced RV systolic function and RA and RV dilation. Her D-dimer was elevated. A CT angiogram of the chest showed bilateral segmental pulmonary emboli (see Figures 1 and 2). Lower extremity deep vein thrombosis studies were negative.
The Pulmonary Embolism Response Team was activated and suggested catheter-directed tissue plasminogen activator (tPA), which the patient refused. She was then started on a heparin drip and transferred to the intensive care unit for closer monitoring. Her hypercoagulable workup results were negative. The patient was bridged to rivaroxaban, and immunosuppressive agents were continued, with significant improvement in clinical status.
Discussion
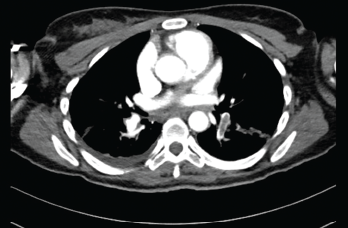
Submassive pulmonary embolism. Filling defects seen in the pulmonary artery.