- A white blood cell count (WBC) of 26×109/L (reference range [RR]: 4.2–10.3×109/L), with 85% neutrophils;
- Hemoglobin (Hgb) at 7.8 g/dL (RR: 11.2–15.7 g/dL);
- Platelets at 361×109/L (RR: 160–383×109/L);
- Aspartate aminotransferase (AST) of 146/L (RR: 10–35/L);
- Alanine transaminase (ALT) of 151/L (RR: 10–35/L); and
- Albumin of 3.2 g/dL (RR: 3.5–5.2 g/dL).
Tests were normal for alkaline phosphatase and bilirubin. Other tests showed:
- An international normalized ratio (INR) of 1.7 (RR 0.9–1.1);
- Lactate dehydrogenase (LDH) at 696 U/L (RR: 135–214 U/L);
- Haptoglobin at 410 mg/dL (RR: 16–200 mg/dL);
- Ferritin at 13,660 ng/mL (RR: 13–150 ng/mL), peaked at 21,000 ng/mL;
- C-reactive protein (CRP) at 23.7 mg/dL (RR: <0.5 mg/dL); and
- An erythrocyte sedimentation rate (ESR) of >130 mm/hr (RR: 0–20 mm/hr).

FIGURES 2A, 2B & 2C (above): Persistent hyperpigmented confluent plaques on the upper thigh, and more linear plaques on the inner thighs and lower leg. (Click to enlarge.)
She had elevated fibrinogen levels. Her creatinine kinase (CK), thyroid stimulating hormone (TSH), creatinine and electrolytes were normal. She also had an unrevealing urinalysis, except a protein count of 100 mg/dL, with a urine protein to creatinine ratio of 0.7.
An evaluation for infectious causes for her condition was negative for syphilis via rapid plasma reagin (RPR), HIV antigen/antibody and RNA, anti-hepatitis A antibody, hepatitis B surface antigen and core antibody IgM/IgG, and anti-hepatitis C antibody, mononucleosis, tuberculosis (T-spot), respiratory viruses, COVID-19, parvovirus B-19, chlamydia and gonorrhea.
One of two initial blood cultures grew Streptococcus mitis/oralis, which was thought to be contaminant. Two repeat blood cultures were negative.
The rheumatology evaluation revealed anti-nuclear antibody (ANA) titers below 1:80. Levels of anti-Jo-1, anti-ribonucleoprotein antibody (RNP), anti-Scl-70 antibody, anti-Smith antibody, anti-SSA antibody (Ro), anti-SSB antibody (La), anti-neutrophil cytoplasmic antibodies (ANCA) and anti-cyclic citrullinated peptide antibody (CCP) were within normal limits. Her rheumatoid factor (RF) was 21 IU/mL (RR: 0–14 IU/mL), and she had an elevated C3 level, with a normal C4.
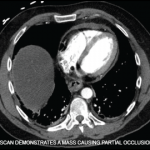
Imaging studies, including chest and knee X-rays and liver ultrasound, were unrevealing, as was echocardiography, without valvular vegetations.
The patient was initially treated empirically with vancomycin and cefepime for possible bacterial infection, which were discontinued after two days following the negative blood cultures.
Skin biopsy pathology reported acanthosis, hyperkeratosis and dyskeratosis in the upper epidermis, consistent with the atypical (persistent) eruption of AOSD.