Pneumatosis cystoides intestinalis (PCI) is a rare gastrointestinal pathological process defined by the presence of gas within the layers of the intestinal wall, commonly within the mucosa and submucosa of the small and large intestines.2,3 PCI has been described in the literature in association with various connective tissue diseases, including scleroderma, mixed connective tissue disease, Sjögren’s disease and systemic lupus erythematosus.1,3 Here, we present a case of PCI in a patient with limited systemic sclerosis.
Clinical Presentation
A 69-year-old woman presented to the rheumatology clinic to establish care. She was diagnosed with limited systemic sclerosis in 2007 by a dermatologist based on sclerodactyly, Raynaud’s phenomenon and telangiectasias. She had never seen a rheumatologist before, nor had she required treatment with any disease-modifying anti-rheumatic drug (DMARD).
She reported a history of gastroesophageal reflux disease and was followed by a gastroenterologist. She denied dysphagia, abdominal pain and distension. She denied any cardiopulmonary symptoms and had no known history of interstitial lung disease or pulmonary hypertension.
Her medical history also included chronic musculoskeletal pain, for which she was treated chronically with ibuprofen and hydrocodone/acetaminophen. She had undergone a partial colectomy in 2011 and was unable to provide any specific reason or diagnosis for this procedure.
Physical examination revealed bilateral sclerodactyly distal to the proximal interphalangeal joints. Multiple telangiectasias were noted on the tongue and the dorsal and ventral aspects of both hands. The cardiac exam did not reveal a murmur. Pulmonary auscultation was notable for crackles at the base of the left lung. Diffuse soft tissue and joint tenderness were noted, without evidence of inflammatory arthritis.
Laboratory testing performed before her appointment revealed an anti-nuclear antibody titer of >1:1280 [reference range: negative] with a centromere pattern.
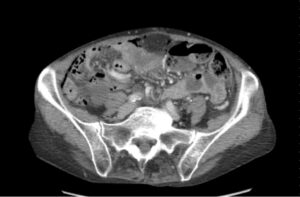
The patient’s abnormal lung exam was evaluated with a two-view chest X-ray. This incidentally revealed pneumoperitoneum (see Figure 1).1
Due to geographic and transportation constraints, the patient was unable to return to the clinic for a repeat evaluation; therefore, she was contacted by telephone. She reported having mild abdominal discomfort and bloating, the nature and duration of which she was not able to clearly describe. She denied any sudden severe abdominal pain, trauma, fever or recent abdominal surgery or procedures. Prompt evaluation at the nearest emergency department was recommended.