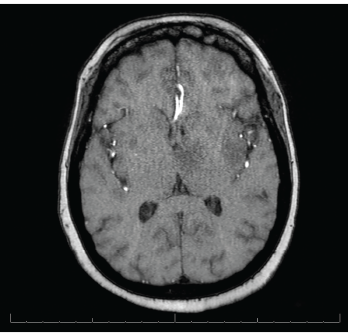
Figure 2. MRI of the brain shows innumerable enhancing lesions scattered throughout the bilateral cerebral and cerebellar hemispheres.
The patient was treated with 1,500 mg of sulfadiazine every six hours, 75 mg of pyrimethamine daily and 25 mg of leucovorin daily, intended for a course of four to six weeks. During her course of treatment, the patient became unresponsive and an emergent head CT revealed a large, left thalamic, intraparenchymal hemorrhage with intraventricular extension causing obstructive hydrocephalus (see Figure 3). A neurosurgeon was consulted.
The patient required intubation and admission to the intensive care unit (ICU). During her ICU stay, the patient had two episodes of tonic-clonic seizures and was started on 500 mg of levetiracetam every 12 hours.
The patient underwent an electroencephalogram, which exhibited diffuse slowing, including frequent generalized rhythmic delta activity, suggesting a moderate degree of bilateral cerebral dysfunction and independent left-hemispheric slowing, temporal maximum, suggesting focal cerebral dysfunction in that region.
Despite aggressive measures, including placement of an external ventricular drain, the neurological status of the patient deteriorated, and the patient died one week following her admission.
The patient’s family declined a brain biopsy.
Discussion
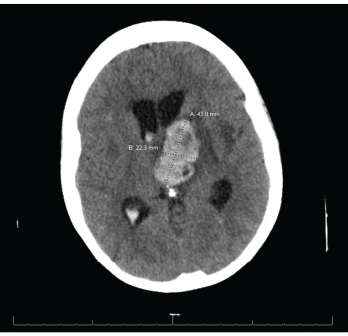
Figure 3. CT reveals a large left thalamic intraparenchymal hemorrhage with intraventricular extension causing obstructive hydrocephalus.
SLE patients are at risk of developing numerous bacterial, viral and parasitic infections secondary to an inherent immunocompromised state.
Opportunistic infections are an established complication of SLE, with an incidence of up to 50%. Studies indicate these infections may involve the skin, nervous system, respiratory system and urinary tract.3-7 One such study, involving more than 33,000 patients with SLE, found an incidence of 10.8 serious infections per 100 person-
years.8 Although the majority of these infections can be attributed to bacteria, viral and parasitic infections are increasingly common, including infections caused by Epstein-Barr virus, human papillomavirus, varicella-zoster virus, cytomegalovirus, parvovirus B19 and the parasite T. gondii.7
Risk factors that predispose SLE patients to infections include being male and Black, longer duration of disease, SLE flare, lupus nephritis, reduction in cell counts (e.g., lymphocytes and neutrophils) and the use of immunosuppressants.7,8 Of note, none of the aforementioned risk factors was present in our patient.
T. gondii is a common opportunistic parasite causing infection in both humans and animals, with the most common course being asymptomatic infection with chronic latency. Neurologic manifestations are commonly seen in congenital infections and immunocompromised patients, and include seizures, hydrocephalus, spasticity, nerve palsies and vision impairment.
The diagnosis of cerebral toxoplasmosis can be established by the presence of a compatible clinical presentation, suggestive brain imaging or detection of T. gondii DNA on polymerase chain reaction of the cerebrospinal fluid.9,10
Although our patient’s clinical presentation was not specific, MRI findings of multiple enhancing lesions, along with an IgG antibody of 145 IU/mL, were highly suggestive of cerebral toxoplasmosis; this diagnosis was subsequently confirmed by PCR of the cerebrospinal fluid, which confirmed the presence of T. gondii. Additionally, the patient’s CRP was elevated at 20 mg/L (normal 0–5 mg/L), also pointing toward an infectious etiology.
Cerebrospinal fluid analysis of the patient in our case report was unremarkable, with no inflammatory changes or pleocytosis. Research suggests cerebrospinal fluid abnormalities are present in 32% of SLE patients with neuropsychiatric illness.11
Additional techniques proposed to elucidate the diagnosis of toxoplasmosis include demonstration of the organism in body fluids or tissues via enzyme-linked immunosorbent assay, rapid electron microscopy, polymerase chain reaction and Wright-Giemsa stained slides.12
A known complication of cerebral involvement in SLE patients is seizures, including grand mal, petit mal, Jacksonian epilepsy and temporal lobe epilepsy.13,14 The patient in question demonstrated seizures of tonic-clonic type. Our patient also developed hydrocephalus, which is frequently associated with cerebral toxoplasmosis.

