Andrew Brookes / Image Source on Offset
Over the past few years, biosimilars and other new drugs have been introduced to treat rheumatic illnesses. Some of the conditions we treat have numerous drug options; others have few or only off-label options. This series, Rheumatology Drugs at a Glance, provides streamlined information on the administration of biologic, biosimilar and other medications used to treat patients with rheumatic disease.
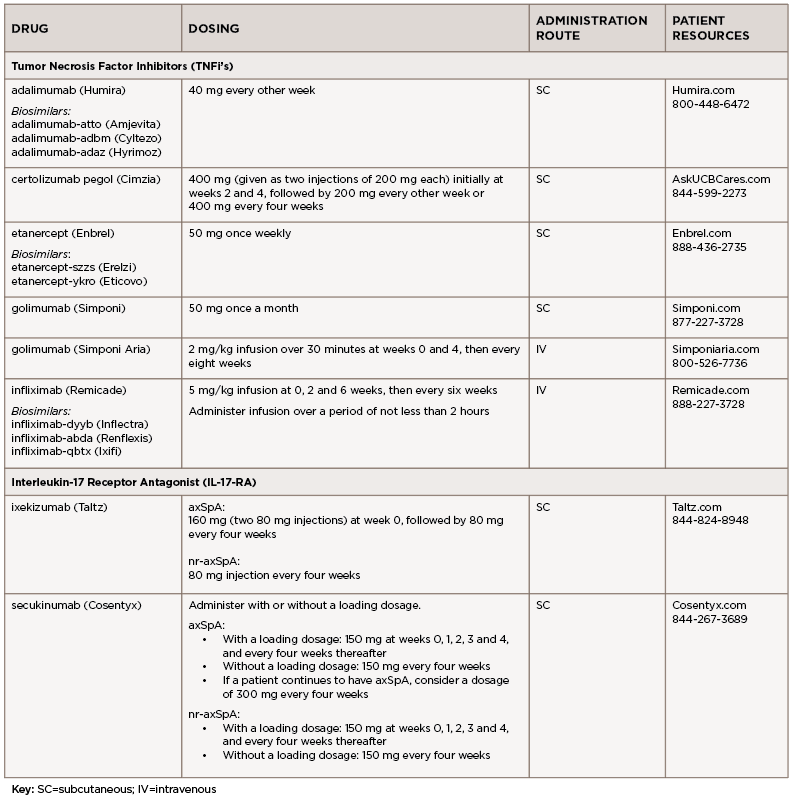
In Part 5 of this series, we discuss the management of axial spondyloarthritis (axSpA), compile insights from three expert clinicians who have achieved distinction in the field of rheumatology and discuss the 16 available options to treat axSpA (see Table 1). The updated ACR axSpA guideline was published in 2019.1
WHAT THE EXPERTS SAY
Lianne S. Gensler, MD, is a professor of medicine at University of California, San Francisco (UCSF), the director of the spondyloarthritis research program and clinic and the program director for the Rheumatology Fellowship Program. Dr. Gensler served as chair of the Spondyloarthritis Research and Treatment Network (SPARTAN) from 2016 to 2018 and currently serves on the executive committee for the Assessment of SpondyloArthritis International Society (ASAS). She has been the recipient of the Ira M. Goldstein Teaching Award in Rheumatology, the Spondylitis Association Young Investigator Award and the UCSF Research Mentoring Award. She has also been inducted into the Council of Master Clinicians at UCSF.
Mark Hwang, MD, is an assistant professor of medicine at the John P. and Kathrine G. McGovern Medical School at the University of Texas Health Science Center at Houston (UTHSC-H). He is a KL2 Scholar in the UTHSC-H Center for Clinical and Translational Sciences KL2 program. He co-directs the UTHSC-H Spondyloarthritis Program in the Division of Rheumatology.
Jean Liew, MD, MS, is an assistant professor of medicine at Boston University School of Medicine and conducts clinical research in osteoarthritis, axial spondyloarthritis and the intersection of COVID-19 with rheumatic disease. As a member of the COVID-19 Global Rheumatology Alliance (GRA) and a member of its steering committee, she is involved in multiple projects relating to data collection, analysis and dissemination of the impact of the COVID-19 pandemic on individuals with rheumatic disease.
Q&A
TR: How do the treatment recommendations differ for axSpA vs. non-radiographic axial spondyloarthritis (nr-axSpA)?

Dr. Gensler
Dr. Gensler: We consider this one disease under the broader, and probably more reliable, term, axial spondyloarthritis (axSpA). The bottom line is the treatment recommendations are the same. The distinction between radiographic axSpA and nr-axSpA is a gray area, technically differentiated by the burden of sacroiliac joint damage (i.e., grade 2 bilaterally or grade 3 or 4 unilaterally) on radiograph. I think the controversy arises for nr-axSpA because these patients have only been studied in trials in the presence of an objective sign of inflammation (e.g., magnetic resonance imaging [MRI] with bone marrow edema and/or elevated C-reactive protein [CRP]). These features may predict response to treatment, so when absent, one should pause and consider whether inflammation is driving disease activity.
There are some non-U.S. Food & Drug Administration (FDA) regulatory agencies that require MRI or CRP elevation in nr-axSpA to receive biologic treatment. Although I do not believe a positive MRI (with bone marrow edema) or elevated CRP is required for treatment, a negative MRI that also has no structural change of the sacroiliac joints—no erosions or subchondral fat—is concerning for the wrong diagnosis, and those patients should be treated with caution.
Dr. Hwang: In terms of axSpA, there is no significant difference in treatment recommendations between axSpA and nr-axSpA to my knowledge. Multiple studies show that regardless of radiographic status, there is a similar severity of disease activity and impact on physical function/health-related quality of life unless there is significant spinal disease. At this time, our current treatment guidelines from the major rheumatology organizations are based on disease activity.
Dr. Liew: For clinical practice, I would say the treatment recommendations (i.e., 2019 ACR/Spondyloarthritis Research and Treatment Network [SPARTAN]/Spondylitis Association of America [SAA] guidelines) don’t differ in terms of what you would actually do. What’s different is the level of evidence: Classification criteria established to identify an nr-axSpA population for studies were not established until about a decade ago. In both radiographic axSpA and nr-axSpA, non-steroidal anti-inflammatory drugs (NSAIDs) are recommended as first-line therapy, and in those who still have active disease despite NSAIDs, then the recommendation is to use tumor necrosis factor (TNF) inhibitors over other biologics.
TR: What are the most common mistakes you see in the management of axSpA?
Dr. Gensler: Hindsight is 20/20, and as healthcare professionals we all approach patients with the same ethos—to try to heal. When I see patients for second opinions, the most common reason the patient is still not doing well is that the diagnosis is not axSpA. I do see patients switched from one biologic to another for pain that is not necessarily driven by ongoing inflammation.